-
 Art of Wellness Acupuncture & Traditional Chinese Medicine (TCM)11704 Wilshire Blvd, Suite 295, Los Angeles, CA, 90025
Art of Wellness Acupuncture & Traditional Chinese Medicine (TCM)11704 Wilshire Blvd, Suite 295, Los Angeles, CA, 90025
myartofwellness@gmail.com310-451-5522 Office Hours
MonClosedTue7:30 am --4 pmWed7:30 am --4 pmThu7:30 am -- 4 pmFri7:30 am -- 4 pmSat7:30 am -- 4 pmSunClosedOur office opens from Tuesdays to Saturdays 7:30 am to 4 pm, will be closed on Memorial day, Independent day, Labor day, Thanksgiving day, Christmas and New year.
-
Recent Posts
- Chinese New Year 2026: Year of the Horse
- Acupuncture and TCM Treatment for Perimenopause Symptoms
- How to Treat Insulin Resistance With Acupuncture and TCM
- How to Treat Metabolic Syndrome With Acupuncture and TCM
- How to Treat Syncope With Acupuncture and TCM
- How to Treat Thoracic Outlet Syndrome With Acupuncture and TCM
- How to Treat Dupuytren’s Contracture With Acupuncture and TCM
- How to Treat Nutcracker Syndrome With Acupuncture and TCM
- How to Treat Rosacea With Acupuncture and TCM
- How to Treat Perioral Dermatitis With Acupuncture and TCM
- Lymphatic Drainage With Acupuncture and TCM
- How to Treat Turf Toe With Acupuncture
- How to Treat Nerve Pain With Acupuncture and TCM
- How to Treat Watery Eyes With Acupuncture and TCM
- How to Treat Ovarian Cysts With Acupuncture and TCM
- How to Treat Dystonia With Acupuncture and TCM
- Sign up to receive news and updates and get my free report:“The Top 10 Reasons to Try Acupuncture”

November 2025 M T W T F S S 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30
Acupuncture
How to Treat Dysmenorrhea With Acupuncture and TCM
By Xiaomei Cai, L.Ac., Ph.D. & Qineng Tan, L.Ac., Ph.D.
Menstrual cramps, unbearable period pain? Severe period cramps and period back pain are dysmenorrhea symptoms. Acupuncture and TCM offer a way to help with cramps and provide period cramp relief.
About 80% of women report having menstrual cramps and painful periods at some point in their lives. Over 40% of women regularly experience PMS cramps, or cramps before period. For some women, the pain is mild enough to tolerate. For others, severe period cramps are truly debilitating, leading to missed days of school or work.
Primary dysmenorrhea is when the period cramps are a result of prostaglandins (hormones) causing the uterus to contract forcefully to expel its lining. For some people, this action leads not only to pelvic pain, but can radiate to cause severe lower back pain, hip pain, or even pain in the legs.
Secondary dysmenorrhea is when severe menstrual cramps are related to another condition, such as endometriosis, uterine fibroids, or pelvic inflammatory disease (PID). About 1 in 10 women between the ages of 15-49 experiences endometriosis, which can cause excruciating pelvic pain during period, and negatively impact fertility. As many as 60-80% of women have fibroids, although many do not know it.
The severe period cramps may feel like a constant ache in the lower abdomen, or more like a gripping or throbbing pain that comes and goes.
Acupuncture and TCM offer an alternative way to treat period cramps and get period pain relief.
Top 5 Dysmenorrhea Symptoms

In addition to menstrual cramps and back pain during the period, some women experience other symptoms of dysmenorrhea, including:
Some women also experience vaginal cramps or ovary pain during period. This may be due to inflammation or scar tissue around the ovaries or ovarian cysts swelling.
How to Help Period Cramps
Generally, doctors will treat dysmenorrhea OTC pain medication, or NSAIDs like Ibuprofen, to relieve menstrual cramping due to primary dysmenorrhea. They may prescribe hormonal birth control, such as oral contraceptives (birth control pills), birth control patch, birth control implant, injection, or vaginal ring.
Hormonal birth control helps relieve period pain because it blocks ovulation and reduces the amount of prostaglandins being produced. However, this medication is not particularly helpful for those who may wish to get pregnant, or those who experience unpleasant side effects from birth control.
Possible Side Effects of Hormonal Birth Control
Many people may find that hormonal birth control causes side effects such as:
Potentially serious side effects may be more common the older a woman is, or the longer she remains on birth control; these could include: blood clots, gallbladder disease, heart disease, or even stroke.
If severe menstrual cramps are not relieved with pain medication, further investigation may be done to determine if there is some other condition causing pelvic pain.
Endometriosis is also usually treated with pain medications and contraceptives, or with Nupron, which suppresses the period. In severe cases, surgery may remove the patches of endometrial tissues. However, with both of these treatments, the endometriosis and severe period pain often come back.
Birth control, pain medications, and even surgeries may temporarily reduce painful cramps, but they are only masking the deeper problems. TCM and acupuncture can help get rid of menstrual cramps because they address the root cause of the pain.
Can Acupuncture Help Get Rid of Period Cramps?

In TCM, we look at organ systems as working together in harmony. Pain usually occurs because there is some imbalance in one or more of the major organ systems. Dysmenorrhea is usually considered to be related to Qi and/or blood stagnation, and often a deficiency of the kidney, liver, or both. In TCM, the liver controls the storage and distribution of blood, so it is central to the process of menstruation.
Dampness and cold are pathogenic forces that can be disruptive to the smooth flow of Qi related to menstruation. Being in a cold, damp place or eating too many cold or damp foods can cause blood stagnation in the abdominal area that leads to painful cramps.
Emotions can also play a significant role, as in TCM we see feelings of anger or depression causing liver stagnation. Deficiency of Qi can happen when a woman has gone through a lot, emotionally and physically, possibly through giving birth, or having stresses put on the reproductive organs.
Scientific research has shown that acupuncture has an effect on the production of key hormones like serotonin, estrogen and progesterone. When we use acupuncture points to balance the function of the liver, kidney, and other organ systems, these chemical changes occur naturally. We also use herbs to get vital nutrients into the blood that we can’t get from food.
Acupuncture is effective for treating conditions like endometriosis, uterine fibroids, ovarian cysts, and PCOS, as well.
Acupuncture treatment and herbal remedies for endometriosis and fibroids have been shown to reduce prostaglandin levels, which helps to relieve painful cramping and also to regulate cycles.
A study of endometriosis patients with dysmenorrhea who received electroacupuncture, the cure rate was 94.4% with low recurrence at the one-year checkup. Another study found that auricular acupuncture was effective 91% for mild to moderate menstrual pain.
TCM herbal formulations have been shown to be highly effective at relieving period pain. They work on the TCM principles of removing blood stasis to reduce swelling and relieve painful cramps.
When we are working to influence the menstrual cycle—in this case, to relieve painful cramping—it is usually best to have acupuncture treatment regularly for about three months. This way, we have time to balance the hormone fluctuations that occur during each phase of the cycle.
Top 3 Tips for Natural Relief from Period Cramps
Your acupuncturist can help give you personalized nutrition advice to help with your unique situation. Most people who are having trouble with painful periods can help themelves by trying these tips:
- Get more Omega-3 fatty acids in your diet – good natural sources include fish, flax seeds, and walnuts. You can also try taking fish oil, cod liver oil, or a vegan omega-3 supplement.
- Reduce consumption of ice-cold foods and beverages – icy drinks, ice cream, and raw foods can all cause a cooling of the uterus, which contributes to painful cramps.
- Avoid mucus-producing foods – foods that are more difficult to digest lead to mucus and stagnation in the organs. Reduce fatty foods, fried foods, and red meat.
Acupuncture Near Me for Dysmenorrhea in Los Angeles, Santa Monica
TCM has been used to treat menstrual difficulties and all types of gynecological issues for many centuries. The doctors at Art of Wellness in West L.A. bring special expertise in both TCM and western medicine gynecology and have partnered with the top women’s health and fertility specialists in Los Angeles. We have over 30 years of experience helping people regulate their menstrual cycles and experience more comfortable periods.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.
How to Treat Diverticulitis With Acupuncture and TCM
By Qineng Tan, L.Ac., Ph.D. and Xiaomei Cai, L.Ac., Ph.D.

Pain in lower left abdomen? Stomach pain or pain in lower abdomen? Nausea, vomiting? Constipation or diarrhea? These may be diverticulitis symptoms. Acupuncture and TCM offer a way to help relieve diverticulitis pain and restore normal bowel function.
Diverticulosis refers to the presence of small sacs or pouches of tissue inside the large intestine, most often the colon (colonic diverticulitis), which are called “diverticula.”
Diverticulitis refers to the condition that occurs when the sacs become inflamed and infected. Diverticulitis causes pain and other symptoms like bloating and pain in left abdomen that might feel better after you pass gas or have a bowel movement.
Diverticular disease is becoming more and more common and is particularly widespread amongst older people, with at least half of all people over the age of 60 showing signs of diverticulosis.
While medical science has not definitively determined why people develop diverticulosis, it is believed to be due to eating a diet that is low in fiber and high in fatty foods like red meat.
Sedentary lifestyle (lack of exercise), being overweight or obese, smoking cigarettes, and regular use of anti-inflammatory medications or OTC pain medications (NSAIDs) may also be factors in the development of diverticulosis.
Many people have diverticulosis but are unaware of it because they don’t have any symptoms. It is only when the diverticula become infected and inflamed that diverticulitis treatment becomes necessary.
Acupuncture and TCM offer an alternative diverticulitis treatment that can help relieve pain and reduce inflammation in the colon.
Top 5 Diverticulitis Symptoms

Diverticulitis symptoms are believed to occur because something like a bit of undigested food or stool becomes trapped inside one of the diverticula, and then bacteria start to grow, causing an infection.
While a person can have diverticulosis for a long time without any signs, symptoms of diverticulitis may come on suddenly and be quite severe.
The common signs of diverticulitis include:
- Abdominal pain or cramping, particularly pain in lower left abdomen—although in Asian countries, pain in lower right abdomen seems to be more prevalent. The pain may be constant, or it can come and go.
- Nausea and/or vomiting
- Fever and/or chills
- Constipation or diarrhea
- Rectal bleeding, bloody stool
Sometimes diverticulitis may cause a total lack of appetite and sudden weight loss, as a person just stops feeling like eating anything.
Diverticulitis can sometimes lead to more serious complications, like an abscess—which is when the infected area swells and fills with pus—or perforation of the bowel wall. These kinds of issues may require surgery.
Diverticulitis Treatment
Some other gastrointestinal disorders can present with symptoms that are similar to those of diverticulitis, such as: colitis or inflammatory bowel disease, IBS (irritable bowel syndrome), or bowel obstruction. Gynecological problems like endometriosis, an ovarian cyst, or an ectopic pregnancy could also cause severe pain in the lower left abdomen. A UTI could also cause acute abdominal pain.
Diagnosis of diverticulitis will usually begin with a doctor feeling the abdomen for signs of tenderness, then they will order tests (blood tests, urine tests, and/or stool tests) to check for infection. Once other problems have been ruled out, a CT scan may show the diverticula (infected sacs/pouches in the large intestine).
There is some debate about when to perform a colonoscopy in cases of diverticulitis, as the procedure can cause perforations of the intestinal lining to become worse. Usually, a colonoscopy is recommended several weeks after a person has recovered from an acute attack of diverticulitis.
Because diverticulitis is usually caused by an infection, the most common medical treatment is a course of antibiotics, along with rest and pain relievers, until the acute symptoms have abated. A liquid diet may be indicated until the situation improves, with the gradual reintroduction of solid foods.
Recommendations will usually include that a person quits smoking (if they smoke) and makes changes in their diet: especially eating less meat and fatty foods and increasing fiber intake. It used to be common for doctors to tell their patients not to eat foods like popcorn, seeds, or nuts, under the assumption that small, hard kernels might become trapped in the diverticula and cause irritation. However, more research has shown that eating these types of foods does not seem to cause flare-ups of diverticulitis.
If these treatments do not help to relieve diverticulitis pain, or if a complication like an abscess or perforation in the colon wall develops, surgery may be necessary. The most common surgery for diverticulitis is a colon resection, which involves removing the part(s) of the large intestine that have been damaged. Sometimes it is not possible to repair the colon completely, and in these cases, a person may have to have a colostomy.
Acupuncture and TCM offer an alternative or adjunct treatment for diverticulitis that can help reduce inflammation in the bowel and relieve abdominal pain.
Can Acupuncture Help Diverticulitis?

An acupuncturist will make a TCM diagnosis based on where and what kind of abdominal pain and other diverticulitis symptoms a patient is experiencing. According to TCM theory, pain and problems with the digestive organs can be related both to stagnant Qi (life energy) or blood in that area, and the presence of a pathogenic force like dampness, heat, or cold.
The quality of diverticulitis pain and how it changes when you eat or move your bowels will provide clues as to what the root cause is.
In TCM, the spleen is considered to be responsible for turning nutrients into energy; when it is not functioning well, a person may have diarrhea. Strengthening the spleen is usually an important part of TCM treatment for diverticulitis and other digestive disorders.
Your acupuncture practitioner can help relieve symptoms like nausea, constipation, diarrhea, bloating, and stomach pain, while also helping to heal and strengthen the lining of the intestines and reducing inflammation. Boosting immune function will help prevent further infections.
It is generally necessary for a person with diverticulosis to make changes in their dietary habits. While increasing intake of fiber and fluids is important, there are probably even more specific foods that are triggering the dysfunction of the gastrointestinal system, creating excess heat or dampness in the internal organs. TCM nutrition views all foods as having properties that either cool or warm the body. So, your acupuncturist will be able to advise you on what food program will work best to balance your health.
In general, nourishing broths, soups, and well-cooked vegetables with lean proteins and whole grains with plenty of fiber are the best diet for people with diverticulitis. Avoid cold, raw foods, fatty foods, red meat, and dairy.
Acupuncture Near Me for Diverticulitis In West Los Angeles
Acupuncture and TCM provide an effective way to treat abdominal pain and gastrointestinal disorders of all kinds. At Art of Wellness, we have over 35 years of experience helping people find pain relief and improve their digestive health.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.
How to Treat Constipation With Acupuncture and TCM
By Xiaomei Cai, L.Ac., Ph.D. & Qineng Tan, L.Ac., Ph.D.

Using a laxative or stool softener so that you can have a bowel movement? Everyone experiences constipation once in a while, but chronic constipation can be a serious issue. Acupuncture and TCM offer a natural way to get constipation relief.
Having difficulty going to the bathroom (pooping) is unfortunately a very common problem. Millions of people see their doctor seeking constipation treatment every year. People of all ages—children, adults, and older people—can suffer from slow digestion and hard bowel movements.
Symptoms of constipation can include:
- Dry, hard stool
- Having less than three bowel movements per week
- Bowel movements are difficult and/or painful
- Bloated stomach
- Abdominal cramps
- Nausea
Basically, constipation occurs when the muscles of the large intestine are not properly moving matter through and out of the colon. Slow movement can result in too much water being absorbed by the colon, causing hard, dry stools.
In general, “normal” bowel movements should be soft and easy to pass, and should happen daily. However, it is not at all uncommon for people to have painful constipation and only go a few times a week, or have even less frequent bowel movements (severe constipation).
There can be many different reasons why there is an imbalance of water in the colon, or that the muscles aren’t functioning well enough. These deeper causes need to be addressed if chronic constipation is becoming an issue.
Fortunately, TCM treatment for constipation includes traditional herb formulations that have been used for centuries as a natural laxative, and acupuncture, which can help strengthen the muscle action of the intestines.
Constipation Causes

Constipation can occasionally occur due to short-term circumstances. Many people experience temporary constipation while they are on a trip and using unfamiliar bathrooms. Eating foods that are unusual for you or low in fiber, becoming dehydrated, not getting any physical activity for several days—these situations could all cause sluggish elimination.
IBS (irritable bowel syndrome), which is considered a functional gastrointestinal disorder, often involves periodic constipation (or diarrhea).
Chronic constipation or severe constipation can have many causes. Sometimes constipation can be caused by a bowel obstruction, or something physically blocking the intestine.
Constipation can also be a secondary condition related to another chronic health problem.
Conditions that cause damage to nerves may disrupt the signals that tell the muscles of the colon to move. These could include:
- Diabetes
- Multiple sclerosis
- Parkinson’s disease
- Stroke
- Injury to the spinal cord
Hormonal imbalances or fluctuations can also lead to constipation. Hormone-related conditions that could contribute to constipation include:
- Diabetes
- Pregnancy
- Menstrual cycle, PMS, Period
- Hypothyroidism
- Hyperparathyroidism
Some medications can cause constipation, such as:
- Narcotics, opioid pain medications (such as Vicodin)
- NSAIDs, like ibuprofen
- Some antidepressants (like Zoloft)
- Blood pressure medications
- Sedatives
- Iron supplements
- Antacids like Maalox or Mylanta
- Diuretics
- Medications for overactive bladder, like Ditropan and Detrol
- Parkinson’s medications, like Sinemet
- Nausea medications
Using laxatives and other over-the-counter constipation remedies as a habit can, unfortunately, perpetuate the cycle and lead to ongoing, chronic constipation.
Mental health conditions like depression and anxiety can also affect regularity. TCM and acupuncture can help improve mental health as well as physical health to help bring constipation relief.
Constipation Side Effects
It is very important to find the root cause of constipation and find a solution. Chronic constipation can lead to other serious complications, such as:
- Hemorrhoids
- Anal fissures
- Diverticulitis
- Fecal impaction
- Stress urinary incontinence
Fortunately, acupuncture and TCM offer natural remedies for constipation without habit-forming medications.
Can Acupuncture Help Relieve Constipation?

In TCM, we diagnose a condition based on the pattern of symptoms each individual person is experiencing, as sometimes the same condition—in this case, constipation—can actually be influenced by many different variables. The diagnostic pattern gives us information about what acupuncture points and herbs will help treat that individual case.
According to TCM theory, constipation can present as:
- Yin Deficiency
- Excess Heat
- Qi Deficiency
In older people, chronic constipation is often related to weakness in the kidneys and liver, which leads to malnourishment and stagnant Qi.
In general, TCM constipation treatment will focus on helping to bring more moisture into the colon and clear heat, while activating the Qi (energy) of the bowel and removing physical and energetic blockages.
Many people who suffer from constipation don’t have enough microbiota or “good bacteria” in their colon. Acupuncture and herbs can help to improve the gut biome.
One study showed that electro-acupuncture helped a significant number of people with chronic constipation have more frequent bowel movements.
One study conducted in China found that, after 20 sessions, gastrointestinal patients who received acupuncture for constipation had a success rate of over 82%, meaning they had more frequent and easier bowel movements.
Another study showed that patients who went through a series of acupuncture treatments sustained longer-lasting efficacy from their treatment than patients who had used medicinal laxatives.
One commonly used Chinese formulation for constipation has been shown to help increase levels of oleamide, which is associated with intestinal motility.
Acupuncture Near Me for Constipation in Los Angeles and Santa Monica
At Art of Wellness, we often treat patients for constipation, whether that is their primary complaint, or sometimes a secondary issue to their other concerns. Acupuncture and Chinese herbs are excellent modalities for helping people achieve regularity and better overall digestion.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.
How to Treat Colitis With Acupuncture and TCM
By Xiaomei Cai, L.Ac., Ph.D. & Qineng Tan, L.Ac., Ph.D.

Diarrhea, bloody stool, fatigue, fever? These could be colitis symptoms. Ulcerative colitis is an inflammatory bowel disease (IBD) that causes swelling in the large intestine, abdominal pain, bloating and bloody diarrhea. Acupuncture and TCM can offer an alternative colitis treatment to help relieve ulcerative colitis symptoms.
Colitis is a gastrointestinal disease in which the colon—also known as the bowel, or the large intestine—becomes inflamed and can develop open sores, or ulcers.
Ulcerative colitis is the term for colitis that is caused by an autoimmune disorder. The immune system launches an attack on the tissues of the intestinal lining, causing inflammation and sores. It is similar to Crohn’s disease: an autoimmune disease that can affect any part of the digestive tract.
What causes colitis? There are several problems that can lead to abdominal pain and diarrhea, and sometimes it can be difficult to discover what is causing a person to have colitis symptoms.
Parasites, bacterial infections, or food poisoning can cause pain, inflammation in the colon, and diarrhea. For example, e coli bacteria, sometimes found in improperly cooked beef, can cause colitis symptoms. This is known as e colitis, or hemorrhagic colitis.
IBS (irritable bowel syndrome) symptoms can seem similar to those of colitis. People who suffer from IBS can have abdominal pain and diarrhea, urgency and mucus in their stool. However, IBS is considered a functional gastrointestinal disorder, not a disease. IBS does not cause permanent damage to the intestinal lining, while colitis can.
Ischemic colitis is a specific type of colitis caused by a blockage of blood flow to the intestine. This is more common in older adults, and can be the result of a blood clot in an artery, or low blood pressure due to heart failure or recovery from some major surgery. Some conditions, like lupus or sickle cell anemia, can restrict blood flow to the gastrointestinal tract. It could also happen due to a bowel obstruction caused by a tumor or hernia. Some medications can also restrict blood flow to the intestine.
TCM and acupuncture treatment, whether alone or as an adjunct to conventional treatment, can help relieve the symptoms of colitis by reducing inflammation in the intestine, helping to stop bleeding and helping to restore normal bowel movements.
Colitis Symptoms

Ulcerative colitis symptoms can be mild at first and become more persistent and/or severe over time. Some common symptoms of colitis, or IBD symptoms, include:
- Loose stool, loose bowel movements, diarrhea
- Urgency to go to the bathroom, feeling like you have to poop all the time
- Feeling like you have to poop, but not being able to
- Bloody stool, bloody poop
- Mucus in stool
- Abdominal pain
- Abdominal cramps, cramping
- Rectal pain
- Fatigue, feeling tired all the time, no energy
- Fever
- Weight loss
Symptoms of ulcerative colitis can come and go, or “flare up” at times. When symptoms abate, this is called “remission.”
Children can have colitis, which may cause them to not grow properly.
Colitis Treatment
Testing for IBDs might start with some basic blood tests and a stool sample test to see if there are any bacterial or parasitic causes of diarrhea. If inflammation needs to be looked at more closely to discover its location and cause, a colonoscopy or sigmoidoscopy may be done. Imaging—X-ray, ultrasound, or MRI—may be used to show if there is some kind of obstruction of the intestine.
If testing and treatment have ruled out IBD and other potential causes, a tissue biopsy may be used to diagnose ulcerative colitis, the autoimmune form of colitis.
Generally, once colitis or inflammatory bowel disease has been diagnosed, the main goal is to reduce inflammation in the colon. Anti-inflammatory drugs will usually be prescribed. Anti-diarrheal medications and pain relievers provide some symptomatic relief.
Ulcerative colitis is usually treated with a combination of anti-inflammatories and immunosuppressants. Unfortunately, these types of medications can have significant side effects. Long term use of corticosteroids can cause bone loss and swelling, while immunosuppressants can stress the liver and pancreas.
Newer pharmacological treatments include “small molecules,” like Xeljanz, which act as anti-inflammatories and immunosuppressants. However, these drugs have been flagged for potentially causing heart problems, and maybe even cancer.
When medications and dietary changes don’t help enough, surgery to remove part of the large intestine may be sought.
Acupuncture and TCM offer an alternative treatment for colitis, which may help relieve symptoms without side effects.
Can Acupuncture Help Colitis?

TCM herbs and acupuncture treatment are excellent modalities for helping to reduce inflammation. In the case of colitis and ulcerative colitis, the central problem is that the body is producing an inflammatory response in the large intestine that leads to pain and dysfunction. According to TCM theory, imbalances in the internal organs can cause heat, dampness, or blood stasis. In different people, the ways that colitis shows up may vary, depending on the pathogenic forces at work.
Acupuncture points to help relieve diarrhea, bloating, and bleeding in the colon will be combined with beneficial herbs to help clear heat and dampness. One study done in China showed that patients with ulcerative colitis who received acupuncture and herbal supplements in addition to conventional pharmaceutical treatments healed more quickly than those who did not receive TCM. They also reported feeling less anxiety and depression.
A systematic review of studies done regarding TCM for colitis concluded that acupuncture and herbs were effective compared to medical treatments.
Studies have shown that acupuncture can help balance the gut biome and help strengthen the intestinal walls.
Acupuncture has been shown to help people whose colitis is in remission to maintain better function.
TCM herbs, used in combination with conventional treatment, may help improve the healing of the mucosal lining of the intestine. One study showed that herbs helped stop bleeding from the colon in patients with ulcerative colitis.
Moxibustion has also been shown to help as a treatment for IBD, helping to relieve diarrhea, nausea, and abdominal cramping.
Acupuncture is believed, in part, to help regulate inflammatory bowel diseases by providing positive stimulation of the vagus nerve, which plays an important role in inflammatory responses.
Acupuncture Near Me for Ulcerative Colitis in Los Angeles and Santa Monica
Acupuncture can be an excellent adjunct to standard treatment for gastrointestinal disorders of all kinds, including: IBS, Crohn’s disease, Celiac disease, and Candida. At Art of Wellness, we have over 30 years of experience helping people with IBD and colitis to improve their quality of life.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.
How to Treat Aphasia With Acupuncture and TCM (Scalp Acupuncture)
By Qineng Tan, L.Ac., Ph.D.
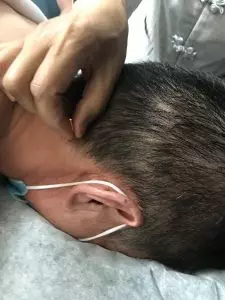
Difficulty speaking, reading or writing due to brain damage is known as “aphasia.” Different types of aphasia can develop after a person has a stroke or head injury. Aphasia can also be a symptom of dementia. Acupuncture—especially “scalp acupuncture”—can help a person regain brain function and speech.
Aphasia—sometimes called “dysphasia”— is a language disorder that occurs because a part of the brain that controls speech, comprehension, and communication is not functioning correctly. This is usually due to damage or pressure on that part of the brain.
Scalp Acupuncture, sometimes called “neuroacupuncture,” is a specific technique that combines Traditional Chinese Medicine and Western medical understanding of neurology. Acupuncture needles are used to stimulate points on the head, or scalp, that have a direct effect on brain cells.
Scalp acupuncture can be helpful in treating acute and chronic central nervous system disorders that cause aphasia, as well as cognitive difficulties, trouble with motor skills, and even paralysis.
Scalp Acupuncture can be used to help people regain brain function after having suffered a stroke or injury to the head. Aphasia is generally considered to be related to this type of damage, but speech problems and trouble with cognition and comprehension can often occur with other neurological disorders, too.
This type of acupuncture treatment can also help people with neurological conditions such as:
- Parkinson’s disease
- Multiple Sclerosis/MS
- Alzheimer’s disease
- Guillain Barre Syndrome
- Ataxia
- Bell’s palsy
- ADD/ADHD
Neurological disorders cause problems with the way the brain communicates information and instructions to the organs and limbs via the nervous system; this is what leads to a wide variety of language and movement disorders.
Scalp acupuncture can be used to help these conditions because it can stimulate malfunctioning brain cells to begin working properly again, encourage the growth of new brain cells, and reestablish connections between the brain and the rest of the central nervous system.
Acupuncture can help improve some of the most common symptoms of neurological disorders like Alzheimer’s, Parkinson’s, and MS, including:
- Aphasia
- Headaches
- Dizziness
- Fatigue
- Mood swings
- Depression
- Muscle spasms, stiff muscles
- Seizures
- Tremor
- Paralysis
Scalp acupuncture can be an effective form of integrative medicine to help people overcome these symptoms, whether they are recovering from a stroke or suffering from a neurological disorder.
What is Scalp Acupuncture?

Acupuncture is one of several modalities used in TCM, which is a complete medical system with a history going back thousands of years. The stimulation of points on the head and/or scalp has always been used as a method for treating all types of symptoms and underlying conditions.
“Scalp acupuncture” is a term that refers to a more specific, contemporary acupuncture technique that combines ancient TCM knowledge with modern medical understanding of the anatomy of the brain and the way parts of the brain interact with the nervous system to control various bodily and sensory functions.
In Chinese Medicine, acupuncture points are usually chosen based on the theory of the meridians—channels along which Qi (energy) moves through the body. Along each meridian lie several points that connect organ systems and parts of the body. This concept of a network system of meridians is more metaphorical in nature, rather than based on actual physiology. In TCM we may consider that a problem in one part of the body is related to an imbalance in a (seemingly) different organ system. For example, anxiety and heart palpitations might be treated by needling a point on the head that is on the Stomach meridian.
In Western medicine, “somatotopic arrangement” describes the understanding of how parts of the brain, and particularly the nerve endings on the scalp, are arrayed in a pattern around the skull and correspond to different sensory functions, such as speech, visual perception, balance, and motor skills. With MRI technology, scientists have been able to “map” out how parts of the nervous system on the scalp correspond to parts of the body, like the feet, and the hands, etc.
With the practice of scalp acupuncture, we are combining these concepts and using acupuncture as a way of directly influencing parts of the brain, like the cerebral cortex, hypothalamus, cerebellum, etc. This can help both to heal parts of the brain that might be damaged due to a stroke, and to regulate functioning of those parts, so as to help restore proper functioning of motor activities and the senses.
This technique involves the insertion of small acupuncture needles into the tissues just beneath the surface of the skin on the scalp. Then, the needles may be be stimulated, either by manually twisting, or with electro-acupuncture (sometimes called “electro-stim”). Here, we attach small electrodes to the needles, and a mild to medium level of electric current flows to activate a vibration and/or rotation.

As part of the goal is to reactivate nervous system connections, the patient may be asked to be active during the treatment; that is, by moving the part of the body that is experiencing weak movement, or at least, to visualize or imagine themselves performing the movement.
One study of patients being treated with scalp acupuncture for aphasia showed that 46% showed “marked improvement,” while almost all patients showed some improvement.
In a study of scalp acupuncture for treatment of paralysis, all patients showed improvement, while 68% were cured.
While more research is needed, it is also believed that scalp acupuncture may be a good alternative therapy to help treat mental health issues, like depression, anxiety, and PTSD, as well as sleep disorders, like insomnia.
Scalp Acupuncture for Aphasia and Stroke Recovery in Los Angeles
At Art of Wellness, we have over 30 years of experience treating neurological disorders of all kinds. Our training in China gave us a thorough understanding of integrative medicine, using both TCM and Western medicine knowledge to provide the best possible outcomes for our patients. We have continued to grow and learn, while working closely with doctors and patients in Los Angeles since 1995. If you or someone you love is recovering from a stroke, or living with a chronic neurological condition, please consider trying acupuncture as an adjunct treatment.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.