-
 Art of Wellness Acupuncture & Traditional Chinese Medicine (TCM)11704 Wilshire Blvd, Suite 295, Los Angeles, CA, 90025
Art of Wellness Acupuncture & Traditional Chinese Medicine (TCM)11704 Wilshire Blvd, Suite 295, Los Angeles, CA, 90025
myartofwellness@gmail.com310-451-5522 Office Hours
MonClosedTue7:30 am --4 pmWed7:30 am --4 pmThu7:30 am -- 4 pmFri7:30 am -- 4 pmSat7:30 am -- 4 pmSunClosedOur office opens from Tuesdays to Saturdays 7:30 am to 4 pm, will be closed on Memorial day, Independent day, Labor day, Thanksgiving day, Christmas and New year.
-
Recent Posts
- How to Treat Rosacea With Acupuncture and TCM
- How to Treat Perioral Dermatitis With Acupuncture and TCM
- Lymphatic Drainage With Acupuncture and TCM
- How to Treat Turf Toe With Acupuncture
- How to Treat Nerve Pain With Acupuncture and TCM
- How to Treat Watery Eyes With Acupuncture and TCM
- How to Treat Ovarian Cysts With Acupuncture and TCM
- How to Treat Dystonia With Acupuncture and TCM
- Can Acupuncture Help Bad Breath?
- How to Treat Atopy with Acupuncture and TCM
- Plantar Fasciosis Treatment With Acupuncture and TCM
- How to Protect Yourself When Air Quality Is Poor
- How to Treat Spinal Headache With Acupuncture and TCM
- How to Treat Sarcoidosis With Acupuncture and TCM
- How to Treat Flu With Acupuncture and TCM
- Chinese New Year 2025 Year of the Snake
- Sign up to receive news and updates and get my free report:“The Top 10 Reasons to Try Acupuncture”

Neurological Conditions
How to Treat Nerve Pain With Acupuncture and TCM
By Qineng Tan, L.Ac., Ph.D. and Xiaomei Cai, L.Ac., Ph.D.
Struggling with sharp, burning, or tingling pain? Do your hands or feet feel numb or hypersensitive? Nerve pain—also called neuropathic pain—can be relieved with acupuncture treatment and other TCM modalities.
Nerve pain occurs when nerves are damaged or dysfunctional, sending incorrect pain signals to the brain. Unlike pain caused by injury or inflammation, nerve pain can persist without an obvious cause and may not respond well to common pain relievers.
Nerve pain can interfere with your ability to work, sleep, or enjoy your day-to-day life. The good news is that acupuncture can be an effective way to treat nerve pain.
What Causes Nerve Pain?
There are many possible underlying conditions that can lead to nerve pain. Here are some of the 10 most most common causes of nerve pain:
- Peripheral neuropathy – often due to diabetes, chemotherapy, or alcohol use
- Trigeminal neuralgia – intense facial pain due to nerve irritation
- Occipital neuralgia – shooting pain at the back of the head and neck
- Cervical radiculopathy – pinched nerves in the neck causing radiating pain
- Carpal tunnel syndrome – pressure on the median nerve in the wrist
- Spinal stenosis or Lumbar stenosis – narrowing of the spinal canal that compresses nerves
- Sciatica – pain radiating down the leg due to sciatic nerve irritation
- Postherpetic neuralgia – lingering nerve pain after shingles
- Dystonia and other movement disorders – can involve nerve dysfunction
- Multiple sclerosis and other autoimmune diseases – affecting nerve conduction
Medical Treatment for Nerve Pain

In Western medicine, the diagnostic process for nerve pain typically begins with a detailed health history and physical examination, focusing on neurological function. Physicians may conduct reflex tests, strength assessments, and evaluate your sensory response. Imaging tests such as MRI or CT scans can help identify structural causes like herniated discs or spinal stenosis. Nerve conduction studies and electromyography (EMG) may be used to assess how well the nerves and muscles are functioning.
Once nerve pain is diagnosed, treatment often involves medications aimed at disrupting the abnormal pain signals. Doctors may prescribe anticonvulsant drugs like gabapentin or pregabalin, which were originally developed to treat epilepsy but are now commonly used to relieve nerve pain.
Certain antidepressants, such as amitriptyline or duloxetine, are also frequently used—not for their mood-enhancing effects, but because they influence how the nervous system processes pain. In some cases, opioids may be prescribed, though they are generally considered a last resort due to the risk of dependence and side effects.
Topical treatments like lidocaine patches or capsaicin cream may offer localized relief for some people. Corticosteroid injections may be recommended if inflammation is contributing to nerve compression, such as in cases of radiculopathy or carpal tunnel syndrome.
Physical therapy can be useful for improving strength, mobility, and nerve function, especially when musculoskeletal imbalances are part of the problem. In more severe cases—such as when a nerve is severely compressed or damaged—surgical intervention may be considered.
While these treatments can sometimes provide temporary relief, they may not address the root cause of nerve dysfunction. Additionally, many patients find that medications come with undesirable side effects or offer only partial relief. That’s why more and more people are turning to acupuncture and Traditional Chinese Medicine (TCM) as a complementary or alternative solution for managing nerve pain holistically.
Can Acupuncture Help Nerve Pain?

In the Western medical model, nerve pain—also called neuropathic pain—is typically understood as the result of damage or dysfunction within the nervous system. This could be due to injury, chronic conditions like diabetes, infections such as shingles, or musculoskeletal issues like spinal stenosis or herniated discs.
TCM, on the other hand, views nerve pain through a holistic lens, focusing on the flow of energy—known as Qi—through the body’s channels or meridians. In this system, pain is often caused by Qi and blood stagnation, which leads to blockages along these pathways. This stagnation can arise from a deficiency in the liver or kidney systems, which in TCM are believed to support and nourish the body’s nerves.
External influences like wind, cold, or dampness may also disrupt the body’s internal balance, leading to symptoms such as numbness, tingling, or sharp, radiating pain. Instead of targeting only the site of discomfort, TCM aims to correct underlying imbalances and restore smooth, harmonious flow throughout the body.
Treatment for nerve pain in TCM often involves acupuncture to stimulate specific points that promote circulation and healing. Herbal medicine is frequently used in combination, with formulas designed to nourish blood, strengthen the liver and kidneys, and dispel pathogenic factors. Other traditional therapies, such as moxibustion (a warming technique using mugwort) or cupping, may be applied to enhance circulation and relieve tension. TCM practitioners also offer guidance on diet, lifestyle, and emotional health to support the body’s natural healing processes and prevent further pain episodes.
A 2023 meta-analysis of 16 studies involving over 1,000 patients with neuropathic pain found that acupuncture significantly reduced pain intensity compared to sham or no treatment.
Acupuncture can modulate receptors and ion channels in peripheral nerves, reducing spontaneous nerve activity that leads to pain.
Studies have shown that acupuncture stimulates the release of neurotrophic factors like nerve growth factor (NGF) and brain-derived neurotrophic factor (BDNF), which support nerve regeneration and repair.
Acupuncture Near Me for Nerve Pain in West Los Angeles
If you’re struggling with nerve pain and looking for a natural, holistic approach to healing, acupuncture and Traditional Chinese Medicine may offer the relief you’ve been hoping for. At Art of Wellness Acupuncture in West Los Angeles, we specialize in helping patients manage complex, chronic pain conditions by addressing the root causes—not just the symptoms. Whether your nerve pain stems from an injury, a chronic condition, or something undiagnosed, we’ll work with you to develop a personalized treatment plan that supports your body’s natural healing processes. Don’t let nerve pain control your life—reach out today to schedule a consultation and take the first step toward lasting relief.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.
How to Treat Dysautonomia With Acupuncture and TCM
By Qineng Tan, L.Ac., Ph.D. and Xiaomei Cai, L.Ac., Ph.D.

Fast heart rate or irregular heartbeat? Feel faint or dizzy when standing up? Fatigue, brain fog? Chest pain? These can all be Dysautonomia symptoms, or autonomic dysfunction. Acupuncture and TCM offer treatment for dysautonomia and autonomic neuropathy.
“Dysautonomia” is a general term that refers to multiple conditions related to autonomic dysfunction. There are many different types of autonomic nervous system disorders that fall under the umbrella of dysautonomia.
The autonomic nervous system (ANS) controls body functions like:
- Blood pressure
- Heart rate
- Breathing
- Digestion
- Temperature regulation
- Urinary function
- Sexual function
- Sweating
Basically, the ANS is in charge of all of the things our bodies do automatically—sometimes called involuntary functions—without us having to think about them.
Dysautonomia symptoms are fairly common, especially later in life, but medical science still has limited options for diagnosing and helping relieve these conditions.
Dysautonomia can be a primary condition, caused by genetic or degenerative disorders, or by damage to nerves (autonomic neuropathy). Secondary dysautonomia can occur as a result of another condition, such as an autoimmune disease, neurological disease, or injury.
Recent studies are beginning to show that dysautonomia, especially POTS, can be linked to long Covid. Even if a person had a Covid infection that was not particularly severe, the long-term effects of the virus have been shown to linger in the body, in the brain and nervous system, causing autonomic dysfunction long after the acute phase of the virus has passed.
TCM offers a way to treat dysautonomia, as acupuncture has been shown to have a positive effect on nervous system function.
Dysautonomia Symptoms
Different types of autonomic dysfunction will cause various symptoms in individuals. The most common symptoms of ANS include:
- Dizziness when standing up or changing position, light-headedness
- Vertigo
- Fainting, passing out
- Arrhythmia, irregular heartbeat, heart palpitations
- Fatigue, feeling tired
- Chest pain
- Shortness of breath
- Trouble swallowing
- Excessive sweating, or lack of sweating, clammy feeling
- Thirst
- Headaches, migraines
- Dry eyes, or excessive tears
- Digestive issues: constipation, diarrhea, etc.
- Frequent urination, incontinence
- Erectile dysfunction (ED)
- Sensitivity to sounds
Top 10 Types of Autonomia

Dysautonomia symptoms can seem similar to those of other nervous system conditions. This is why it can be difficult to be correctly diagnosed. It is fairly common for a person presenting with symptoms of dysautonomia to be told that they are suffering from anxiety or panic disorder.
Secondary dysautonomia occurs when another condition is the cause of symptoms. For example, dysautonomia systems can be the result of having disorders, such as:
- Parkinson’s disease
- Ehlers-Danlos Syndrome
- Celiac disease
- Guillain-Barre syndrome
- Lupus
- Lyme disease
- Sjogren’s syndrome
- Ulcerative Colitis
- Multiple Sclerosis (MS)
- Rheumatoid arthritis
- Sarcoidosis
- Crohn’s Disease
- IBS
- Fibromyalgia
These conditions can all cause damage to parts of the autonomic nervous system and therefore lead to symptoms of Dysautonomia.
There are at least 15 different types of Primary Dysautonomia. POTS is probably the most common one.
POTS Postural Orthostatic Tachycardia Syndrome – POTS is a condition characterized by an excessive increase in heart rate when moving from lying down to standing up (orthostatic intolerance). Symptoms may include lightheadedness, palpitations, fatigue, and fainting. It often affects young adults, particularly women.
Hyperadrenergic POTS is a subtype of POTS characterized by excessive sympathetic nervous system activity, leading to symptoms such as palpitations, anxiety, tremors, and hypertension in addition to orthostatic intolerance.
Treatment for POTS often involves a combination of lifestyle modifications, medications, and physical therapy. Lifestyle changes may include increasing fluid and salt intake to expand blood volume, wearing compression stockings to prevent blood pooling in the legs, and gradually increasing physical activity to improve cardiovascular fitness. Medications such as beta-blockers, fludrocortisone, midodrine, and pyridostigmine may be prescribed to help regulate heart rate, blood pressure, and blood volume.
IST Inappropriate Sinus Tachycardia – Inappropriate Sinus Tachycardia (IST) is a condition characterized by a fast heart rate at rest that is not caused by exercise, fever, or stress. It is considered inappropriate because the heart rate is elevated without a physiological reason. People with IST typically experience heart rates exceeding 100 beats per minute while at rest, often accompanied by symptoms such as palpitations, chest discomfort, fatigue, and shortness of breath.
The exact cause of IST is not fully understood, but it is believed to involve dysfunction in the sinus node, the natural pacemaker of the heart, which regulates heart rate. In individuals with IST, the sinus node may become overly sensitive to normal stimuli, leading to excessive firing and a rapid heart rate.
Treatment for IST focuses on controlling symptoms and improving quality of life. Lifestyle modifications like stress reduction, regular exercise, and avoiding triggers such as caffeine and nicotine may be recommended. Medications such as beta-blockers, calcium channel blockers, or ivabradine may be prescribed to help slow the heart rate and alleviate symptoms. In severe cases that do not respond to medication, procedures such as catheter ablation may be considered to modify the electrical pathways in the heart and reduce symptoms.
NCS Neurocardiogenic Syncope or Vasovagal Syncope – NCS, also known as vasovagal syncope, is a form of dysautonomia characterized by a sudden drop in heart rate and blood pressure, leading to fainting. It can be triggered by various factors such as prolonged standing, emotional stress, or pain.
Management of NCS focuses on avoiding triggers like prolonged standing, dehydration, or emotional stress, which can lead to fainting episodes. Increasing fluid and salt intake may help prevent episodes by expanding blood volume. Medications such as beta-blockers or fludrocortisone may be prescribed to help stabilize heart rate and blood pressure. In severe cases, implantation of a pacemaker or other cardiac device may be considered to regulate heart rhythm.
AAG Autoimmune Autonomic Ganglionopathy – AAG is a rare autoimmune disorder characterized by the production of antibodies that target autonomic ganglia, leading to autonomic dysfunction. Symptoms may include orthostatic hypotension, gastrointestinal dysmotility, and urinary dysfunction.
MSA Multiple System Atrophy – Management of MSA is focused on addressing specific symptoms related to autonomic dysfunction, parkinsonism, and cerebellar ataxia. Medications such as levodopa-carbidopa may be prescribed to alleviate motor symptoms, while medications such as fludrocortisone or midodrine may be used to manage orthostatic hypotension. Physical therapy and speech therapy may also be beneficial for managing motor and speech difficulties associated with MSA.
Management of MSA is focused on addressing specific symptoms related to autonomic dysfunction, parkinsonism, and cerebellar ataxia. Medications such as levodopa-carbidopa may be prescribed to alleviate motor symptoms, while medications such as fludrocortisone or midodrine may be used to manage orthostatic hypotension. Physical therapy and speech therapy may also be beneficial for managing motor and speech difficulties associated with MSA.
PAF Pure Autonomic Failure – PAF is a rare condition characterized by dysfunction of the autonomic nervous system, leading to problems with blood pressure regulation, heart rate variability, and temperature control. Symptoms may include orthostatic hypotension, urinary retention, and gastrointestinal issues.
Treatment for PAF aims to manage symptoms related to autonomic dysfunction. Lifestyle modifications like elevating the head of the bed, wearing compression garments, and increasing fluid and salt intake may help alleviate symptoms of orthostatic hypotension. Medications such as midodrine, fludrocortisone, and droxidopa may be prescribed to raise blood pressure and improve symptoms.
FD Familial Dysautonomia – begins at birth as a result of a genetic mutation inherited from the parents. FD affects the central nervous system, breathing, digestion, ability to form tears, regulation of temperature, regulation of blood pressure, taste, and pain sensitivity. Usually diagnosed in infancy, as babies will have trouble with feeding, will not cry tears, and will show poor growth. As the disease progresses, there may be development of arrhythmia, GERD, dry eyes and vision problems, scoliosis and/or weak bones.

DBHD Dopamine-Beta Hydrolase Deficiency – a rare genetic disorder characterized by the body’s inability to produce the enzyme dopamine-beta hydroxylase (DBH). This enzyme is essential for converting dopamine to norepinephrine, a neurotransmitter involved in regulating blood pressure and other autonomic functions.
Treatment for DBH deficiency focuses on managing symptoms by increasing fluid and salt intake to help maintain blood pressure, wearing compression garments to reduce symptoms of orthostatic hypotension, and avoiding triggers such as hot environments and prolonged standing.
In some cases, medications that increase blood volume or constrict blood vessels may be prescribed to help alleviate symptoms. However, treatment options for DBH deficiency are limited, and management typically involves ongoing monitoring and adjustment of therapies to address specific symptoms and complications as they arise.
OI Orthostatic Intolerance – Orthostatic intolerance (OI) refers to a group of conditions characterized by symptoms such as lightheadedness, dizziness, fatigue, and fainting when a person moves from lying down into an upright position.
There are various types of orthostatic intolerance, including postural orthostatic tachycardia syndrome (POTS), neurally mediated hypotension (NMH), and vasovagal syncope. Each type presents with its own set of symptoms and underlying mechanisms.
Besides lifestyle modifications such as increasing fluid and salt intake, wearing compression garments, and engaging in regular exercise can help improve blood flow and cardiovascular function, medications such as beta-blockers, fludrocortisone, and midodrine may also be prescribed to help regulate heart rate and blood pressure.
BF Baroreflex Failure – Baroreflex failure is a condition characterized by the inability of the body to regulate blood pressure in response to changes in posture or stress. It can result in symptoms such as orthostatic hypotension, hypertension, and fluctuations in heart rate.
Can Acupuncture Help Dysautonomia?

From the perspective of conventional medicine, dysautonomia is still considered a mysterious, confusing problem to solve. But TCM philosophy has recognized this type of disorder for many centuries. Acupuncture has been used since ancient times to help regulate the autonomic nervous system, although we have not always used that terminology for it.
A Chinese medical text that dates back to the first century B.C.E. describes “Ying-Wei Disharmony,” the symptoms of which include: breathing dysfunction, palpitations, irregular heartbeat, anxiety, digestive problems, nausea, dizziness, chronic pain, pressure headaches, tingling and numbness (neuropathy), and insomnia.
For a long time, medical science has looked for the mechanisms that make acupuncture work.
Recent studies have begun to show more clearly that the stimulation of acupoints affects the neural pathways, including the autonomic nervous system.
Acupuncture has been shown to help regulate ANS functions such as temperature regulation, blood pressure, heart rate, and muscle sympathetic nerve activities.
Acupuncture helps modulate transmitters in the brain, restoring balance when these activities have become dysregulated. More specifically, electro-acupuncture has been shown to work upon the hypothalamus, the medulla oblongata, the dorsomedial prefrontal cortex, and other regions of the brain that contribute to ANS function.
One study involving 30 female patients with dysautonomia symptoms showed that acupuncture treatment helped relieve heart palpitations, abdominal issues, and helped patients sleep better.
In addition to helping to regulate the autonomic nervous system, an acupuncturist will look for signs that other organ systems are out of balance and contributing to symptoms. For example, some patients with dysautonomia may need acupuncture and herbs to help balance the spleen and kidneys, which will in turn help improve adrenal function.
Stagnation of blood or phlegm can sometimes be causing blockages that contribute to nervous system dysfunction.
Acupuncture Near Me for Dysautonomia in Los Angeles Area
Dysautonomia is a complex condition to treat. A multi-faceted approach, combining conventional medical approaches with medications with acupuncture and herbal remedies can be helpful for managing the variety of symptoms a person may be experiencing. TCM is an excellent modality for working with this type of condition. If you or someone you know is struggling to get help for POTS or other autonomic disorders, call us at Art of Wellness in West L.A..
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.
How to Treat POTS With Acupuncture and TCM
By Qineng Tan, L.Ac., Ph.D. and Xiaomei Cai, L.Ac., Ph.D.

Do you often feel shaky, like you’re fainting, or experience dizziness, especially when you’re getting up from sitting down or lying down? Do you feel like you have a rapid heartbeat, or shortness of breath? Postural orthostatic tachycardia syndrome, known as PoTS syndrome, or POTS, is a condition that causes unstable blood pressure when changing positions. Acupuncture and TCM can help relieve dizziness and other symptoms of POTS.
Postural tachycardia syndrome (or postural orthostatic tachycardia syndrome) is a chronic disorder related to the autonomic nervous system that causes people to experience dizziness and increased heart rate when they move into an upright position; this is known as orthostatic intolerance, which is a type of dysautonomia.
POTS syndrome is fairly common, affecting up to 3 million people in the U.S. POTS occurs more often in people assigned female at birth, and often first shows up during the teenage years.
The most common symptom of POTS is feeling light-headed when changing your position from sitting to standing, or when getting up from lying down.
Whenever we have been sitting or lying down for a while, blood pools in the lower parts of the body. When we get up, the autonomic nervous system starts a series of actions to move blood back up into the top half of the body. This involves squeezing blood vessels, and releasing adrenaline and norepinephrine, to make the heart beat faster.
When a person has POTS, more blood tends to pool in the legs, and the nervous system process doesn’t cause the normal, quick response from the blood vessels, so more hormones are released, which can cause the person’s heart rate to increase, and a dizzy, faint feeling.
Medical science has not yet discovered exactly what causes POTS, but there are different characteristics that allow for categorizing these different types of POTS syndrome:
- Neuropathic POTS – damage to small fiber nerves that control blood vessel constriction in the abdomen and limbs
- Hyperadrenergic POTS – when a person has elevated levels of norepinephrine
- Hypovolemic POTS – when a person has unusually low blood levels
- Secondary POTS – when POTS symptoms are related to another condition that causes neuropathy, such as Lyme disease, diabetes, or autoimmune disorders like Lupus or celiac disease.
While POTS is not rare, it can be difficult to get a diagnosis, because the criteria can be vague, and the symptoms can so often be related to other conditions, or just seem “normal.”
For many people, POTS is truly debilitating and can have a serious, negative impact on daily life. It can also contribute to feelings of anxiety and depression. Acupuncture and TCM offer an adjunct or alternative treatment for POTS that can help with dizziness, irregular heartbeat, digestive problems, muscle weakness, migraines, trouble sleeping, and other symptoms, all at the same time.
Top 10 POTS Symptoms
The primary symptoms of POTS are related to the cardiovascular system: rapid heartbeat, and dizziness. However, there can be many other POTS symptoms.
- Irregular heart rate, rapid heart rate, fast heartbeat, chest pain, heart palpitations
- Dizziness, especially when standing up or getting up from lying down, feeling faint
- Breathing problems: hyperventilating, bronchial asthma, shortness of breath
- Constipation, diarrhea, nausea, abdominal pain
- Muscle weakness, muscle pain, tremor
- Skin rash, flushed face, flushing, sweating
- Migraine headaches
- Cognitive issues, brain fog, difficulty concentrating
- Trouble sleeping
- Frequent urination, nocturia

Other symptoms of POTS may include: tinnitus (ringing in the ears), blurred vision, red or purple appearance of the legs when standing up, and a “jittery” feeling or general nervousness.
As with many syndromes, different people will experience different combinations of symptoms. While dizziness and rapid heartbeat are the signs most commonly associated with POTS, many people with POTS will also suffer from abdominal pain and gastrointestinal problems, perhaps without realizing there is a correlation.
POTS symptoms may resemble many other conditions, such as:
- Chronic fatigue syndrome, ME/CFS
- Graves disease
- Other heart conditions that involve tachycardia
- Anemia
- Stroke
- Epilepsy
- Adrenal fatigue
- Drug use
- Eating disorders
- Benign paroxysmal positional vertigo
- Ménière’s disease
Because POTS is often misunderstood or misdiagnosed, many patients will be offered medications to manage headaches, vertigo, or depression, which may not offer much relief.
Medical Treatment for POTS
As there is no definitive cure for POTS, Postural orthostatic tachycardia syndrome treatments typically aim to manage symptoms and improve quality of life.
Dietary modifications are a fundamental component of POTS management. Adequate daily fluid intake is crucial. A diet that includes plenty of salt helps maintain blood volume, aiding blood flow to vital organs. Patients are typically advised to avoid alcohol and carefully monitor caffeine intake, as these substances can exacerbate symptoms.
Exercise is gradually introduced, often starting in reclined or horizontal positions, with the goal of increasing exercise tolerance over time. Physical therapy helps retrain the autonomic nervous system, enhancing blood circulation.
Compression garments can help reduce blood pooling, and specific postures while sitting or sleeping may alleviate symptoms. Identifying triggers such as prolonged sitting, heat, or certain drugs allows for better symptom control. Regular monitoring of blood pressure and pulse, along with adequate sleep hygiene, aids overall well-being.
While no single pharmacological solution is universally effective, some medications may be prescribed based on individual symptoms. These may help to improve blood volume, aid sodium retention, reduce heart rate, and enhance blood vessel constriction.
While POTS symptoms may intermittently improve with medications and lifestyle modifications, the underlying cause of POTS may persist. Acupuncture and TCM treatment can provide a holistic solution for individuals living with POTS, which may help to address the root causes of this syndrome.
Can Acupuncture Help POTS?

POTS is a kind of Dysautonomia; this is a general term that describes conditions that involve malfunctioning of the autonomic nervous system. This causes people’s bodies to have problems with regulating the sorts of functions that are typically automatic, like the beating of the heart, circulation of blood, breathing, and temperature control.
Western medicine offers some treatments that can help address individual symptoms of dysautonomia, but it does not have a way of treating the root of the problem. It can be difficult to get proper treatment, because people who suffer from POTS and other kinds of dysautonomia often seem reasonably healthy, and their complaints—dizziness, headaches, mental health problems—seem vague.
Acupuncture and TCM have been used to treat these kinds of problems for centuries. Acupuncture treatment can help provide positive effects on the subtle communications of the nervous system, as well as the heart rate, and physiological symptoms of anxiety. According to TCM theory, several organ systems may be involved and need support: not only the heart, but also the kidneys or spleen.
Studies have shown that acupuncture for dysautonomia can help relieve symptoms like heart palpitations, insomnia, and digestive problems.
A qualified acupuncturist is also well-versed in nutrition and can offer more detailed information regarding dietary and lifestyle changes that can help each individual patient. Your TCM provider will spend time learning more about you, so that they can offer personalized advice.
Acupuncture Near Me for POTS in West Los Angeles
TCM and acupuncture can help people with all types of autoimmune disorders, nerve disorders, and conditions involving fatigue and dizziness that may be difficult to solve with conventional methods. Acupuncture works on a deeper, more subtle level to help address complex syndromes. If you are regularly experiencing trouble with feeling light-headed, having unexplained headaches and sleep problems, it may be time to seek a more holistic alternative treatment.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.
How to Treat CRPS With Acupuncture and TCM
By Qineng Tan, L.Ac., Ph.D. and Xiaomei Cai, L.Ac., Ph.D.

Chronic pain, changes in skin temperature, and swelling in a specific limb or body part? Pain, swollen limbs, edema and inflammation after a seemingly minor injury? These could be signs of a condition known as Complex Regional Pain Syndrome (CRPS). Acupuncture and TCM can help relieve chronic pain due to CRPS.
CRPS is a relatively rare condition that usually causes pain and inflammation in an arm or leg. It most often occurs after someone experiences an injury to a limb, or has surgery on one of their limbs. The painful area may be swollen, turn red and hot sometimes, and blue and cold at other times.
CRPS is marked by pain that seems disproportionate to the injury or outside stimulus. For example, a person with CRPS may feel severe pain when the affected area is touched lightly, or when a breeze blows. While CRPS is not fully understood by medical science, it is generally considered to be a neurological disorder.
While most cases of CRPS do improve in the long run, there may be a long period of time during which the injured area seems to be getting more inflamed.
CRPS pain may worsen and spread to involve more of the affected limb. In some cases, the pain may even be “mirrored” in the opposite limb. This is partially why CRPS is theorized to be caused by problems with the nervous system.
Sometimes CRPS manifests without any evidence of nerve damage. This condition is known as CRPS-I, or Reflex Sympathetic Dystrophy Syndrome. (RSD or RSDS).
Some cases of CRPS can be associated with proven nerve damage; this is called “causalgia,” or CRPS-II.
Conventional Western medicine approaches primarily focus on managing symptoms with pain medications and physical therapy. In some cases, CRPS pain can be so severe that it causes disability, as the person cannot use their limb normally in daily activities.
Traditional Chinese Medicine (TCM) and acupuncture can help address the root causes of CRPS. Acupuncture and TCM offer a holistic approach to relieve pain and enhance overall well-being.
Top 5 Symptoms of Complex Regional Pain Syndrome (CRPS)

CRPS symptoms can change. A CRPS flare up may last days or weeks, when pain and swelling get worse. Sometimes, the pain may seem to come out of nowhere; other times, it may be triggered by exertion, stress, or other factors.
- Intense and prolonged pain: Individuals with CRPS experience severe and persistent pain that may seem disproportionate to the initial injury or cause. There may be “pins and needles” or a burning sensation. Light contact with something may cause severe pain; this phenomenon is known as “allodynia.” Or something that would usually cause mild pain, like a pin prick, causes severed pain; this is called “hyperalgesia.”
- Changes in skin temperature and color: The affected area may become warmer or cooler compared to the surrounding areas, and skin may appear blotchy, pale, red, or blue or gray.
- Swelling and sensitivity: Swelling, edema, and increased sensitivity to touch or even a slight breeze are common symptoms of CRPS.
- Limited range of motion: Stiffness, muscle weakness, and difficulty moving the affected limb or body part may occur. There may be tremors or jerky motions of the limb.
- Changes in skin texture, hair and nail growth: Abnormal hair and nail growth patterns, such as excessive hair growth or brittle nails, may develop in the affected area. The skin may become thinner or thicker, or may be shiny or scaly.
CRPS may cause unusually heavy sweating in the affected area, or cause there to be a total absence of sweating in the area.
Medical Treatment for CRPS
In the realm of conventional medicine, Complex Regional Pain Syndrome (CRPS) is understood as a multifaceted condition that often arises following an injury or trauma to a limb or body part. While the exact cause of CRPS is not fully understood, it is believed to involve abnormal responses of the central and peripheral nervous systems. Nerve damage, inflammation, and changes in blood flow are thought to play a role in the development of CRPS.
Certain risk factors may increase an individual’s susceptibility to the condition, such as a history of fractures, surgery, or repetitive motion injuries. Additionally, psychological factors and genetic predisposition may contribute to the development of CRPS.
CRPS can be triggered by a variety of factors, including surgery, immobilization, infections, emotional stress and trauma.
Diagnostic testing for CRPS may include a bone scan, x-rays, MRI, and a sweat production test.
Medications recommended may include pain relievers, corticosteroids to help bring down inflammation, and nerve blocking injections. Low doses of ketamine are sometimes used to help relieve pain. Topical analgesics may help reduce sensitivity in the affected area, as may heat therapy.
Other therapies for CRPS may include biofeedback and transcutaneous electrical nerve stimulation (TENS). Mirror therapy, in which a person stands or sits in front of a mirror set-up that tricks the brain into thinking it sees the injured limb working the way the healthy limb does, can be helpful for retraining the nervous system.
Acupuncture treatment for CRPS can work on multiple levels to help relieve pain, improve motor function, reduce inflammation, help heal nerves, and reduce stress.
Can Acupuncture Help CRPS?

In Traditional Chinese Medicine (TCM), Complex Regional Pain Syndrome (CRPS) is understood as a disruption in the flow of Qi (energy) and Blood in the affected area, leading to pain and dysfunction. According to TCM theory, the underlying causes of CRPS are often related to the stagnation of Qi and Blood, as well as the blockage of meridians (energy channels) that run through the affected limb or body part. TCM treatments aim to restore the smooth flow of Qi and Blood, harmonize the body’s internal balance, and alleviate pain.
Acupuncture, a key component of TCM, is believed to stimulate specific acupoints along the meridians, helping to regulate the nervous system’s response and promote healing. Chinese herbal medicine is also commonly used in TCM to support the treatment of CRPS by addressing underlying imbalances and promoting overall well being. By addressing both the physical and energetic aspects of the condition, TCM aims to restore harmony and alleviate pain in individuals with CRPS.
One study looked at two soldiers whose upper extremities were injured in combat and were later diagnosed with CRPS. When conventional methods did not help relieve pain, they were given one or two acupuncture treatments per week for a few weeks. They had 80% improvement in pain and functionality and with no recurrence at a 20-month follow up.
An individual case study of a 34-year-old with CRPS showed improvement in pain and emotional well-being after a series of acupuncture treatments.
When dealing with Complex Regional Pain Syndrome (CRPS), incorporating certain lifestyle changes, behavioral adjustments, dietary modifications, and home remedies can be beneficial in managing the condition. Here are some recommendations:
Stress Management: Practicing stress-reducing techniques such as deep breathing exercises, meditation, and mindfulness can help alleviate CRPS symptoms. Stress management techniques promote relaxation and can positively impact pain perception.
- Gentle Exercise: Engaging in low-impact exercises like walking, swimming, or yoga can help improve blood circulation, maintain joint flexibility, and reduce muscle stiffness. It is important to consult with a healthcare professional or physical therapist to determine the most appropriate exercise program for your specific situation.
- Heat and Cold Therapy: Applying heat packs or cold compresses to the affected area may provide temporary relief from pain and inflammation. Experiment with both methods to see which works best for you. Remember to protect your skin and avoid extreme temperatures.
- Balanced Diet: Maintaining a healthy and well-balanced diet is crucial for overall well-being. Include nutrient-rich foods such as fruits, vegetables, whole grains, lean proteins, and healthy fats. Avoid excessive consumption of processed foods, refined sugars, and caffeine, as they may contribute to inflammation and worsen symptoms.
- Adequate Hydration: Staying hydrated is important for promoting optimal bodily function and supporting overall health. Aim to drink an adequate amount of water throughout the day to keep your body hydrated and support proper circulation.
- Stress Reduction: CRPS symptoms can be exacerbated by stress. Engaging in activities that promote relaxation, such as hobbies, listening to soothing music, spending time in nature, or engaging in creative outlets, can help reduce stress levels and improve overall well-being.
- Sleep Hygiene: Getting sufficient and quality sleep is essential for managing chronic pain conditions. Establish a regular sleep routine, create a comfortable sleep environment, and practice good sleep hygiene habits like avoiding electronic devices before bed.
It’s important to note that these lifestyle changes, behavioral adjustments, dietary modifications, and home remedies should complement your comprehensive treatment plan and be tailored to your individual needs. Consult with a healthcare professional or a qualified practitioner of Traditional Chinese Medicine (TCM) for personalized guidance and recommendations based on your specific condition and symptoms.
Acupuncture Near Me for CRPS in Los Angeles and Santa Monica
At Art of Wellness Acupuncture in West L.A., we have over 35 years of experience treating neurological conditions and chronic pain of all kinds. Acupuncture is a modality that is particularly suited to treating conditions like CRPS, where it may be difficult to find relief through conventional treatment methods. If you are experiencing excessive pain in one of your limbs, with temperature sensitivity and inflammation, it may be worth seeking out alternative treatment with TCM.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.
How to Treat Aphasia With Acupuncture and TCM (Scalp Acupuncture)
By Qineng Tan, L.Ac., Ph.D.
Difficulty speaking, reading or writing due to brain damage is known as “aphasia.” Different types of aphasia can develop after a person has a stroke or head injury. Aphasia can also be a symptom of dementia. Acupuncture—especially “scalp acupuncture”—can help a person regain brain function and speech.
Aphasia—sometimes called “dysphasia”— is a language disorder that occurs because a part of the brain that controls speech, comprehension, and communication is not functioning correctly. This is usually due to damage or pressure on that part of the brain.
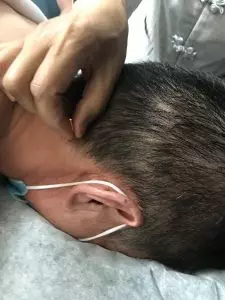
Scalp Acupuncture, sometimes called “neuroacupuncture,” is a specific technique that combines Traditional Chinese Medicine and Western medical understanding of neurology. Acupuncture needles are used to stimulate points on the head, or scalp, that have a direct effect on brain cells.
Scalp acupuncture can be helpful in treating acute and chronic central nervous system disorders that cause aphasia, as well as cognitive difficulties, trouble with motor skills, and even paralysis.
Scalp Acupuncture can be used to help people regain brain function after having suffered a stroke or injury to the head. Aphasia is generally considered to be related to this type of damage, but speech problems and trouble with cognition and comprehension can often occur with other neurological disorders, too.
This type of acupuncture treatment can also help people with neurological conditions such as:
- Parkinson’s disease
- Multiple Sclerosis/MS
- Alzheimer’s disease
- Guillain Barre Syndrome
- Ataxia
- Bell’s palsy
- ADD/ADHD
Neurological disorders cause problems with the way the brain communicates information and instructions to the organs and limbs via the nervous system; this is what leads to a wide variety of language and movement disorders.
Scalp acupuncture can be used to help these conditions because it can stimulate malfunctioning brain cells to begin working properly again, encourage the growth of new brain cells, and reestablish connections between the brain and the rest of the central nervous system.
Acupuncture can help improve some of the most common symptoms of neurological disorders like Alzheimer’s, Parkinson’s, and MS, including:
- Aphasia
- Headaches
- Dizziness
- Fatigue
- Mood swings
- Depression
- Muscle spasms, stiff muscles
- Seizures
- Tremor
- Paralysis
Scalp acupuncture can be an effective form of integrative medicine to help people overcome these symptoms, whether they are recovering from a stroke or suffering from a neurological disorder.
What is Scalp Acupuncture?

Acupuncture is one of several modalities used in TCM, which is a complete medical system with a history going back thousands of years. The stimulation of points on the head and/or scalp has always been used as a method for treating all types of symptoms and underlying conditions.
“Scalp acupuncture” is a term that refers to a more specific, contemporary acupuncture technique that combines ancient TCM knowledge with modern medical understanding of the anatomy of the brain and the way parts of the brain interact with the nervous system to control various bodily and sensory functions.
In Chinese Medicine, acupuncture points are usually chosen based on the theory of the meridians—channels along which Qi (energy) moves through the body. Along each meridian lie several points that connect organ systems and parts of the body. This concept of a network system of meridians is more metaphorical in nature, rather than based on actual physiology. In TCM we may consider that a problem in one part of the body is related to an imbalance in a (seemingly) different organ system. For example, anxiety and heart palpitations might be treated by needling a point on the head that is on the Stomach meridian.
In Western medicine, “somatotopic arrangement” describes the understanding of how parts of the brain, and particularly the nerve endings on the scalp, are arrayed in a pattern around the skull and correspond to different sensory functions, such as speech, visual perception, balance, and motor skills. With MRI technology, scientists have been able to “map” out how parts of the nervous system on the scalp correspond to parts of the body, like the feet, and the hands, etc.
With the practice of scalp acupuncture, we are combining these concepts and using acupuncture as a way of directly influencing parts of the brain, like the cerebral cortex, hypothalamus, cerebellum, etc. This can help both to heal parts of the brain that might be damaged due to a stroke, and to regulate functioning of those parts, so as to help restore proper functioning of motor activities and the senses.
This technique involves the insertion of small acupuncture needles into the tissues just beneath the surface of the skin on the scalp. Then, the needles may be be stimulated, either by manually twisting, or with electro-acupuncture (sometimes called “electro-stim”). Here, we attach small electrodes to the needles, and a mild to medium level of electric current flows to activate a vibration and/or rotation.

As part of the goal is to reactivate nervous system connections, the patient may be asked to be active during the treatment; that is, by moving the part of the body that is experiencing weak movement, or at least, to visualize or imagine themselves performing the movement.
One study of patients being treated with scalp acupuncture for aphasia showed that 46% showed “marked improvement,” while almost all patients showed some improvement.
In a study of scalp acupuncture for treatment of paralysis, all patients showed improvement, while 68% were cured.
While more research is needed, it is also believed that scalp acupuncture may be a good alternative therapy to help treat mental health issues, like depression, anxiety, and PTSD, as well as sleep disorders, like insomnia.
Scalp Acupuncture for Aphasia and Stroke Recovery in Los Angeles
At Art of Wellness, we have over 30 years of experience treating neurological disorders of all kinds. Our training in China gave us a thorough understanding of integrative medicine, using both TCM and Western medicine knowledge to provide the best possible outcomes for our patients. We have continued to grow and learn, while working closely with doctors and patients in Los Angeles since 1995. If you or someone you love is recovering from a stroke, or living with a chronic neurological condition, please consider trying acupuncture as an adjunct treatment.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.