-
 Art of Wellness Acupuncture & Traditional Chinese Medicine (TCM)11704 Wilshire Blvd, Suite 295, Los Angeles, CA, 90025
Art of Wellness Acupuncture & Traditional Chinese Medicine (TCM)11704 Wilshire Blvd, Suite 295, Los Angeles, CA, 90025
myartofwellness@gmail.com310-451-5522 Office Hours
MonClosedTue7:30 am --4 pmWed7:30 am --4 pmThu7:30 am -- 4 pmFri7:30 am -- 4 pmSat7:30 am -- 4 pmSunClosedOur office opens from Tuesdays to Saturdays 7:30 am to 4 pm, will be closed on Memorial day, Independent day, Labor day, Thanksgiving day, Christmas and New year.
-
Recent Posts
- How to Treat Chronic Kidney Disease (CKD) With Acupuncture and TCM
- How to Treat Edema With Acupuncture and TCM
- How to Treat Cirrhosis With Acupuncture and TCM
- How to Treat SIBO With Acupuncture and TCM
- How to Treat Pruritus With Acupuncture and TCM
- How to Treat MCAS With Acupuncture and TCM
- How to Treat Shin Splints With Acupuncture and TCM
- How to Treat Dysautonomia With Acupuncture and TCM
- How to Treat Myofascial Pain Syndrome With Acupuncture and TCM
- How to Treat Costochondritis With Acupuncture and TCM
- How to Treat Ankylosing Spondylitis With Acupuncture and TCM
- How to Treat Gastroparesis With Acupuncture and TCM
- Sign up to receive news and updates and get my free report:“The Top 10 Reasons to Try Acupuncture”

Anxiety
How to Treat Pruritus With Acupuncture and TCM
By Xiaomei Cai, L.Ac., Ph.D. and Qineng Tan, L.Ac., Ph.D.

Itchy skin, hives all over the body, or skin rashes that itch? Pruritus, commonly known as itching, is an irritating and persistent condition that affects many people. Acupuncture and TCM herbs can offer a holistic approach to alleviate itching.
Pruritus is simply a medical term that means “itching,” or that feeling that you need to scratch your skin. It can refer to itchy skin on one part of the body, or systemic itching that feels like it moves around or affects the whole body. The sensation can be mild, even ticklish, or painful and constant to the point that it is debilitating.
The sensation of itching all over body can significantly impact one’s quality of life, as it can be painful, distracting, and make it difficult to concentrate, relax, or sleep.
Persistent itching requires treatment that takes many possible underlying factors into consideration. This is why acupuncture and TCM can be a good alternative treatment for pruritus.
What Causes Pruritus?
Pruritus can stem from various causes. It can be a primary condition, arising due to a skin problem or skin allergy, such as:
- Atopic dermatitis
- Dermatitis herpetiformis
- Psoriasis
- Eczema
- Hives, urticaria
- Folliculitis
- Dry skin
- Hemorrhoids
- Head lice infestation
Pruritus can also be caused by many other conditions, such as nerve damage, renal disorders that require dialysis, blood diseases like polycythemia vera, hepatitis, liver cirrhosis, infections like chicken pox and shingles, HIV, thyroid disorders, MCAS, pregnancy and perimenopause.
Top 10 Pruritus Causes
Because the sensation of itching, like that of pain, can be influenced by so many factors, there are many possible causes of pruritus. Itchy skin can be caused by a wide variety of conditions, including:
- Allergic Reactions: Common allergens include certain foods, medications, and insect stings or bites. Immune system disorders like MCAS can cause pruritus.
- Dermatitis: Conditions like atopic dermatitis (eczema) and contact dermatitis can lead to persistent itching.
- Skin Infections: Bacterial, viral, and fungal infections can cause itching.
- Dry Skin (Xerosis): Often exacerbated by environmental factors, dry skin can cause itching.
- Internal Diseases: Liver disease, chronic kidney disease, thyroid problems, and certain cancers can cause systemic itching. Chronic kidney disease that require dialysis treatment, in particular, can cause a condition known as Uremic Pruritus.
- Nervous System Disorders: Conditions such as multiple sclerosis, pinched nerves, and postherpetic neuralgia can lead to pruritus. Brachioradial pruritus, for example, is a condition in which irritation of the cervical nerves (C5-C8) causes itching on one or both of the the upper arms.
- Mental Health Issues: Stress, anxiety, and obsessive-compulsive disorder can manifest with itching.
- Pregnancy: Some women experience pruritus during pregnancy due to hormonal changes.
- Perimenopause: Some women experience pruritus during perimenopause and menopause due to a reduction in estrogen levels.
- Reactions to medications: Many drugs can cause pruritus as a side effect, including antibiotics like penicillin, amoxicillin, erythromycin, blood pressure medications, statins, or cholesterol medications, analgesics like aspirin, and tricyclic antidepressants.
Treatment for Pruritus

Conventional medicine typically treats pruritus by trying to find and address the underlying cause, while using medications to alleviate the symptom of itching. This may include topical treatments like over-the-counter or prescription creams and ointments that contain corticosteroids, menthol, or capsaicin to soothe the skin and reduce inflammation. These creams may help relieve localized itching for a time, but they cannot do much to control widespread, systemic itching.
Antihistamines, such as diphenhydramine or cetirizine, may be prescribed to reduce allergic reactions and relieve itching. These can be helpful in some acute cases of pruritus, but again, they do not resolve the problem of chronic itching. Overall, most people with chronic pruritus do not get adequate relief from antihistamine treatment for itching.
For severe itching, oral corticosteroids or immunosuppressants may be prescribed to reduce inflammation and immune response.
TCM and acupuncture can be an effective alternative or adjunct treatment for itching, as TCM addressed both underlying conditions and the symptoms of itchy skin.
Can Acupuncture Help Pruritus?
TCM methods like acupuncture and moxibustion have been used for over 2000 years to help relieve itchy skin conditions and systemic pruritus. Now, scientific research is beginning to show that Chinese medicine is an effective alternative treatment for itching.
The mechanisms that cause the sensation of itching often stem from the brain and the peripheral nervous system. Acupuncture has been shown to have an effect on the nervous system, and specifically, to help reduce the activation of the itch response in the brain.
Itching responses are also activated by the behavior of mast cells, like cytokines. Acupuncture, particularly electroacupuncture, has been shown to help regulate the activity of cytokines, which can help reduce inflammation and sensation.
Acupuncture is well known, now, to help relieve pain by stimulating receptors in the brain. This same action can help to reduce itchy sensations, as well as pain.
The chemical and mechanical activations that cause itching can lead to a chronic problem referred to as the “itch-scratch vicious cycle,” which occurs because of a neural loop in the spinal cord. Acupuncture can potentially help to disrupt this chronic loop of activations that causes the urge to scratch.

Acupuncture and TCM herbal remedies can also help to clear up skin conditions that are directly causing itching, and can help to address deeper underlying conditions, such as liver and kidney ailments, that can be the secondary cause of systemic itching.
Uremic pruritus, which is associated with dialysis treatment for chronic kidney disease or renal failure, affects many people. This type of pruritus can cause sleep problems and affect patients on a daily basis and is believed to be caused by severe dryness of the skin, along with sweating, and chronic inflammation. It may also be related to opioid receptors and inappropriate nerve signaling that triggers the release of cytokines. A review of studies about acupuncture treatment for chronic kidney disease suggests that TCM is highly effective for reducing itching related to uremic pruritus.
One specific study looked at patients undergoing dialysis who were given acupressure treatment. The conclusion was that acupressure was both helpful for relieving itching and cost effective as a treatment alternative.
Acupuncture treatment has an impact not only on the autonomic nervous system, but also on histamine release, and studies have shown that acupuncture is more effective at controlling histamine-related itching than many antihistamine medications.
One study done with 16 patients suffering from brachioradial pruritus (itching on the upper arm/s) found that the majority experienced total resolution of their itching, while the remaining patients experienced partial relief of itching.
Acupuncture Near Me for Pruritus in West Los Angeles
Acupuncture can be beneficial for itchy skin conditions like hives, dermatitis, and rashes. During pregnancy and perimenopause, acupuncture can help balance hormones to relieve itching and insomnia. Acupuncture can also help relieve anxiety, PTSD and panic disorders that can sometimes exacerbate itching sensations. Liver problems, kidney problems, and side effects of cancer treatment can all be addressed with TCM, which may help relieve persistent pruritus.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.
How to Treat Dysautonomia With Acupuncture and TCM
By Qineng Tan, L.Ac., Ph.D. and Xiaomei Cai, L.Ac., Ph.D.

Fast heart rate or irregular heartbeat? Feel faint or dizzy when standing up? Fatigue, brain fog? Chest pain? These can all be Dysautonomia symptoms, or autonomic dysfunction. Acupuncture and TCM offer treatment for dysautonomia and autonomic neuropathy.
“Dysautonomia” is a general term that refers to multiple conditions related to autonomic dysfunction. There are many different types of autonomic nervous system disorders that fall under the umbrella of dysautonomia.
The autonomic nervous system (ANS) controls body functions like:
- Blood pressure
- Heart rate
- Breathing
- Digestion
- Temperature regulation
- Urinary function
- Sexual function
- Sweating
Basically, the ANS is in charge of all of the things our bodies do automatically—sometimes called involuntary functions—without us having to think about them.
Dysautonomia symptoms are fairly common, especially later in life, but medical science still has limited options for diagnosing and helping relieve these conditions.
Dysautonomia can be a primary condition, caused by genetic or degenerative disorders, or by damage to nerves (autonomic neuropathy). Secondary dysautonomia can occur as a result of another condition, such as an autoimmune disease, neurological disease, or injury.
Recent studies are beginning to show that dysautonomia, especially POTS, can be linked to long Covid. Even if a person had a Covid infection that was not particularly severe, the long-term effects of the virus have been shown to linger in the body, in the brain and nervous system, causing autonomic dysfunction long after the acute phase of the virus has passed.
TCM offers a way to treat dysautonomia, as acupuncture has been shown to have a positive effect on nervous system function.
Dysautonomia Symptoms
Different types of autonomic dysfunction will cause various symptoms in individuals. The most common symptoms of ANS include:
- Dizziness when standing up or changing position, light-headedness
- Vertigo
- Fainting, passing out
- Arrhythmia, irregular heartbeat, heart palpitations
- Fatigue, feeling tired
- Chest pain
- Shortness of breath
- Trouble swallowing
- Excessive sweating, or lack of sweating, clammy feeling
- Thirst
- Headaches, migraines
- Dry eyes, or excessive tears
- Digestive issues: constipation, diarrhea, etc.
- Frequent urination, incontinence
- Erectile dysfunction (ED)
- Sensitivity to sounds
Top 10 Types of Autonomia

Dysautonomia symptoms can seem similar to those of other nervous system conditions. This is why it can be difficult to be correctly diagnosed. It is fairly common for a person presenting with symptoms of dysautonomia to be told that they are suffering from anxiety or panic disorder.
Secondary dysautonomia occurs when another condition is the cause of symptoms. For example, dysautonomia systems can be the result of having disorders, such as:
- Parkinson’s disease
- Ehlers-Danlos Syndrome
- Celiac disease
- Guillain-Barre syndrome
- Lupus
- Lyme disease
- Sjogren’s syndrome
- Ulcerative Colitis
- Multiple Sclerosis (MS)
- Rheumatoid arthritis
- Sarcoidosis
- Crohn’s Disease
- IBS
- Fibromyalgia
These conditions can all cause damage to parts of the autonomic nervous system and therefore lead to symptoms of Dysautonomia.
There are at least 15 different types of Primary Dysautonomia. POTS is probably the most common one.
POTS Postural Orthostatic Tachycardia Syndrome – POTS is a condition characterized by an excessive increase in heart rate when moving from lying down to standing up (orthostatic intolerance). Symptoms may include lightheadedness, palpitations, fatigue, and fainting. It often affects young adults, particularly women.
Hyperadrenergic POTS is a subtype of POTS characterized by excessive sympathetic nervous system activity, leading to symptoms such as palpitations, anxiety, tremors, and hypertension in addition to orthostatic intolerance.
Treatment for POTS often involves a combination of lifestyle modifications, medications, and physical therapy. Lifestyle changes may include increasing fluid and salt intake to expand blood volume, wearing compression stockings to prevent blood pooling in the legs, and gradually increasing physical activity to improve cardiovascular fitness. Medications such as beta-blockers, fludrocortisone, midodrine, and pyridostigmine may be prescribed to help regulate heart rate, blood pressure, and blood volume.
IST Inappropriate Sinus Tachycardia – Inappropriate Sinus Tachycardia (IST) is a condition characterized by a fast heart rate at rest that is not caused by exercise, fever, or stress. It is considered inappropriate because the heart rate is elevated without a physiological reason. People with IST typically experience heart rates exceeding 100 beats per minute while at rest, often accompanied by symptoms such as palpitations, chest discomfort, fatigue, and shortness of breath.
The exact cause of IST is not fully understood, but it is believed to involve dysfunction in the sinus node, the natural pacemaker of the heart, which regulates heart rate. In individuals with IST, the sinus node may become overly sensitive to normal stimuli, leading to excessive firing and a rapid heart rate.
Treatment for IST focuses on controlling symptoms and improving quality of life. Lifestyle modifications like stress reduction, regular exercise, and avoiding triggers such as caffeine and nicotine may be recommended. Medications such as beta-blockers, calcium channel blockers, or ivabradine may be prescribed to help slow the heart rate and alleviate symptoms. In severe cases that do not respond to medication, procedures such as catheter ablation may be considered to modify the electrical pathways in the heart and reduce symptoms.
NCS Neurocardiogenic Syncope or Vasovagal Syncope – NCS, also known as vasovagal syncope, is a form of dysautonomia characterized by a sudden drop in heart rate and blood pressure, leading to fainting. It can be triggered by various factors such as prolonged standing, emotional stress, or pain.
Management of NCS focuses on avoiding triggers like prolonged standing, dehydration, or emotional stress, which can lead to fainting episodes. Increasing fluid and salt intake may help prevent episodes by expanding blood volume. Medications such as beta-blockers or fludrocortisone may be prescribed to help stabilize heart rate and blood pressure. In severe cases, implantation of a pacemaker or other cardiac device may be considered to regulate heart rhythm.
AAG Autoimmune Autonomic Ganglionopathy – AAG is a rare autoimmune disorder characterized by the production of antibodies that target autonomic ganglia, leading to autonomic dysfunction. Symptoms may include orthostatic hypotension, gastrointestinal dysmotility, and urinary dysfunction.
MSA Multiple System Atrophy – Management of MSA is focused on addressing specific symptoms related to autonomic dysfunction, parkinsonism, and cerebellar ataxia. Medications such as levodopa-carbidopa may be prescribed to alleviate motor symptoms, while medications such as fludrocortisone or midodrine may be used to manage orthostatic hypotension. Physical therapy and speech therapy may also be beneficial for managing motor and speech difficulties associated with MSA.
Management of MSA is focused on addressing specific symptoms related to autonomic dysfunction, parkinsonism, and cerebellar ataxia. Medications such as levodopa-carbidopa may be prescribed to alleviate motor symptoms, while medications such as fludrocortisone or midodrine may be used to manage orthostatic hypotension. Physical therapy and speech therapy may also be beneficial for managing motor and speech difficulties associated with MSA.
PAF Pure Autonomic Failure – PAF is a rare condition characterized by dysfunction of the autonomic nervous system, leading to problems with blood pressure regulation, heart rate variability, and temperature control. Symptoms may include orthostatic hypotension, urinary retention, and gastrointestinal issues.
Treatment for PAF aims to manage symptoms related to autonomic dysfunction. Lifestyle modifications like elevating the head of the bed, wearing compression garments, and increasing fluid and salt intake may help alleviate symptoms of orthostatic hypotension. Medications such as midodrine, fludrocortisone, and droxidopa may be prescribed to raise blood pressure and improve symptoms.
FD Familial Dysautonomia – begins at birth as a result of a genetic mutation inherited from the parents. FD affects the central nervous system, breathing, digestion, ability to form tears, regulation of temperature, regulation of blood pressure, taste, and pain sensitivity. Usually diagnosed in infancy, as babies will have trouble with feeding, will not cry tears, and will show poor growth. As the disease progresses, there may be development of arrhythmia, GERD, dry eyes and vision problems, scoliosis and/or weak bones.

DBHD Dopamine-Beta Hydrolase Deficiency – a rare genetic disorder characterized by the body’s inability to produce the enzyme dopamine-beta hydroxylase (DBH). This enzyme is essential for converting dopamine to norepinephrine, a neurotransmitter involved in regulating blood pressure and other autonomic functions.
Treatment for DBH deficiency focuses on managing symptoms by increasing fluid and salt intake to help maintain blood pressure, wearing compression garments to reduce symptoms of orthostatic hypotension, and avoiding triggers such as hot environments and prolonged standing.
In some cases, medications that increase blood volume or constrict blood vessels may be prescribed to help alleviate symptoms. However, treatment options for DBH deficiency are limited, and management typically involves ongoing monitoring and adjustment of therapies to address specific symptoms and complications as they arise.
OI Orthostatic Intolerance – Orthostatic intolerance (OI) refers to a group of conditions characterized by symptoms such as lightheadedness, dizziness, fatigue, and fainting when a person moves from lying down into an upright position.
There are various types of orthostatic intolerance, including postural orthostatic tachycardia syndrome (POTS), neurally mediated hypotension (NMH), and vasovagal syncope. Each type presents with its own set of symptoms and underlying mechanisms.
Besides lifestyle modifications such as increasing fluid and salt intake, wearing compression garments, and engaging in regular exercise can help improve blood flow and cardiovascular function, medications such as beta-blockers, fludrocortisone, and midodrine may also be prescribed to help regulate heart rate and blood pressure.
BF Baroreflex Failure – Baroreflex failure is a condition characterized by the inability of the body to regulate blood pressure in response to changes in posture or stress. It can result in symptoms such as orthostatic hypotension, hypertension, and fluctuations in heart rate.
Can Acupuncture Help Dysautonomia?

From the perspective of conventional medicine, dysautonomia is still considered a mysterious, confusing problem to solve. But TCM philosophy has recognized this type of disorder for many centuries. Acupuncture has been used since ancient times to help regulate the autonomic nervous system, although we have not always used that terminology for it.
A Chinese medical text that dates back to the first century B.C.E. describes “Ying-Wei Disharmony,” the symptoms of which include: breathing dysfunction, palpitations, irregular heartbeat, anxiety, digestive problems, nausea, dizziness, chronic pain, pressure headaches, tingling and numbness (neuropathy), and insomnia.
For a long time, medical science has looked for the mechanisms that make acupuncture work.
Recent studies have begun to show more clearly that the stimulation of acupoints affects the neural pathways, including the autonomic nervous system.
Acupuncture has been shown to help regulate ANS functions such as temperature regulation, blood pressure, heart rate, and muscle sympathetic nerve activities.
Acupuncture helps modulate transmitters in the brain, restoring balance when these activities have become dysregulated. More specifically, electro-acupuncture has been shown to work upon the hypothalamus, the medulla oblongata, the dorsomedial prefrontal cortex, and other regions of the brain that contribute to ANS function.
One study involving 30 female patients with dysautonomia symptoms showed that acupuncture treatment helped relieve heart palpitations, abdominal issues, and helped patients sleep better.
In addition to helping to regulate the autonomic nervous system, an acupuncturist will look for signs that other organ systems are out of balance and contributing to symptoms. For example, some patients with dysautonomia may need acupuncture and herbs to help balance the spleen and kidneys, which will in turn help improve adrenal function.
Stagnation of blood or phlegm can sometimes be causing blockages that contribute to nervous system dysfunction.
Acupuncture Near Me for Dysautonomia in Los Angeles Area
Dysautonomia is a complex condition to treat. A multi-faceted approach, combining conventional medical approaches with medications with acupuncture and herbal remedies can be helpful for managing the variety of symptoms a person may be experiencing. TCM is an excellent modality for working with this type of condition. If you or someone you know is struggling to get help for POTS or other autonomic disorders, call us at Art of Wellness in West L.A..
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.
How to Treat Chronic Fatigue Syndrome With Acupuncture and TCM
By Xiaomei Cai, L.Ac., Ph.D. & Qineng Tan, L.Ac., Ph.D.
Chronic fatigue syndrome (CFS), also known as myalgic encephalitis (ME/CFS), is a condition marked by extreme fatigue that doesn’t get better, even with rest, and gets worse with physical and mental exertion. Chronic fatigue is not well understood by medical science, but acupuncture and Chinese medicine for chronic fatigue syndrome symptoms can be an effective treatment option.
People with chronic fatigue syndrome are always tired, even after getting a normal amount of sleep, and the condition persists for weeks, months, or years. Other chronic fatigue symptoms include body aches, cognitive problems, vision problems, and emotional or mental health problems, like depression and anxiety.
If a person feels tired all the time, with no medical explanation, for six months or more, and has several other chronic fatigue syndrome symptoms like dizziness, difficulty concentrating, headaches, or sensitivity to light, then they might be diagnosed with CFS, or myalgic encephalitis (ME CFS).
By definition, a syndrome is a collection of symptoms that often appear together in combination, for which the exact explanation is unknown. Chronic fatigue has been considered a syndrome for some time, but has more recently been given the designation of a “disease;” hence, the newer term “myalgic encephalitis,” which refers to muscle pain and inflammation of the brain and spinal cord.
Chronic fatigue syndrome symptoms can be very similar to those of fibromyalgia. People with fibromyalgia also experience severe fatigue, but the primary symptoms of fibromyalgia are musculoskeletal pain that comes and goes all over, especially in “tender points” around the major muscles and joints, along with swelling and inflammation. It is possible to have both ME/CFS and fibromyalgia.
Women are much more likely to have chronic fatigue than men. MECFS can begin to appear at any stage of life, but most usually develops in adulthood. It is estimated that up to 90% of people who have chronic fatigue go undiagnosed.
ME/CFS is a serious and disabling condition that can interfere with even the most basic daily activities. People with chronic fatigue may be able to participate in some events where they exert themselves mentally and/or physically, but afterwards, they will feel completely wiped out and have to take time to recover, often confined to bed. This is called post-exertional malaise (PEM).
Top 10 Chronic Fatigue Syndrome Symptoms
The most common ME/CFS symptoms include:
- Fatigue, tired all the time, weakness
- Sensitivity to light
- Trouble concentrating, hard to focus, memory problems, confusion
- Dizziness, especially when getting up from lying down
- Headaches
- Muscle aches, body ache, muscle weakness, joint pain
- Enlarged lymph nodes in neck or armpit area, sore throat
- Tired after exercise or mental exertion (post-exertional malaise)
- Depression, mood swings, moodiness
- Insomnia, sleep problems
Other signs of chronic fatigue syndrome may include: fever, abdominal pain, weight loss or weight gain, allergies, rash, rapid heart beat, and night sweats/hot flashes.
What Causes Chronic Fatigue?
The cause of ME/CFS is not known. Immune system dysfunction, the aftereffects of having a virus, and psychological factors have all been associated with the development of chronic fatigue.
Some people begin to have symptoms of chronic fatigue after having a viral infection, such as Epstein Barr, mononucleosis, or herpes. Postural orthostatic tachycardia syndrome (POTS) is also strongly associated with chronic fatigue.
While it does seem that some people who suffer from CFS also have immune system problems, chronic fatigue is not considered to be an autoimmune disorder in and of itself. As with other conditions like lupus or fibromyalgia, CFS sometimes appears after a person has gone through some sort of emotional trauma or physical injury.
Some people with chronic fatigue have hormone imbalances related to pituitary hormone, adrenal hormone, or hypothalamus hormones, but it is not understood how these might be related to their condition. Diabetes, anemia, or hypothyroidism can also create hormonal imbalances that can contribute to chronic fatigue.
In some cases, chronic fatigue could be due to a sleep disorder, such as sleep apnea or chronic insomnia. Long-standing mental health issues like depression, anxiety, or PTSD can interfere with sleep and hormone responses, contributing to the chronic fatigue syndrome symptoms.
Treatment for Chronic Fatigue Syndrome Symptoms

There is no clear treatment protocol within conventional Western medicine for ME/CFS. A doctor may diagnose myalgic encephalitis if they have ruled out other possibilities and then try to recommend medications or various types of therapy to help people deal with the symptoms of chronic fatigue.
Pain relievers or NSAIDs will often be the standard recommendation for handling ME/CFS related pain like headaches or muscles aches.
Doctors may prescribe antidepressants as a way of helping patients cope with depression and anxiety related to chronic fatigue. However, these medications can sometimes cause side effects that will exacerbate the chronic fatigue rather than helping it.
Some doctors have tried treating CFS with antiviral medications, corticosteroids, or thyroid hormone medications. None of the pharmacological interventions that have been used to treat chronic fatigue syndrome have proved to be very effective.
Thus, many patients with ME/CFS consider turning to alternative medicine or complementary therapies to relieve CFS symptoms. Acupuncture is now widely recognized as an alternative therapy for chronic fatigue.
Can Acupuncture and Chinese Medicine Help Chronic Fatigue Syndrome?
Traditional Chinese medicine is well suited to treatment for ME/CFS. Overall, TCM philosophy pays close attention to the subtle balance of energy, known as Qi, within the body as a whole, as well as within the various organ systems. By observing the specific symptoms each person experiences as part of chronic fatigue syndrome, we can pinpoint which organ systems are deficient and need strengthening.
Classic TCM patterns related to chronic fatigue diagnosis include:
- Spleen Qi deficiency
- Liver Qi stagnation
- Kidney deficiency
- Yin deficiency
- Heat toxicity
- Phlegm obstruction/dampness
Latent heat and dampness are sometimes the long-term effects of a viral infection or other illness, or a long period of emotional stress. These conditions originate from an external pathogenic factor, but then cause a series of imbalances which weaken the kidneys and other organs over time. Acupuncture treatment and herbs can help reduce inflammation and strengthen Qi.
A TCM doctor will choose acupuncture points and a combination of herbs that will help harmonize the affected systems. With herbs, we are able to get nutrients into the body beyond what you can do with foods alone. A balanced diet that cools heat and tonifies the organs will also be important for recovering strength and energy.
One controlled trial found that four weeks of acupuncture treatment led to improvements in CFS symptoms.
A systematic review of studies regarding acupuncture treatment for ME CFS showed a reduction in the severity of fatigue.
A study using acupuncture and moxibustion treatment for CFS showed a 90% effective rate, with half of the patients feeling that their CFS was “cured.”
Another study involving acupuncture and moxibustion found that the moxa treatment in particular became more and more effective as treatment sessions continued past the 10th treatment. Moxibustion was shown to have an effect on the vagus nerve, which controls the parasympathetic nervous system.
How long it takes to get results from acupuncture treatment for chronic fatigue will vary from person to person, depending on how long the person has been experiencing CFS, and how deeply the organ systems are affected. TCM treatment has a cumulative effect which strengthens over time and several sessions.
Acupuncture Near Me for Chronic Fatigue Syndrome (ME/CFS) in the Los Angeles Area
ME CFS is far more common than statistics show, because many people suffer in silence and invisibility. Now, many people are struggling with chronic fatigue after having COVID-19. TCM modalities like acupuncture, Chinese herbs, and moxibustion, can help relieve fatigue, depression, mental fogginess, poor sleep, and other symptoms of CFS. If you or someone you love has been feeling exhausted for months without improvement, it may be time to consider trying acupuncture for chronic fatigue.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.
How To Treat Claustrophobia Anxiety Disorder With Acupuncture and TCM
By Xiaomei Cai, L.Ac., Ph.D. & Qineng Tan, L.Ac., Ph.D.

Claustrophobia is a specific kind of anxiety disorder in which fear of being in an enclosed space can bring on symptoms similar to those of panic attacks. Claustrophobic feelings like being anxious, hyperventilating, sweating, shaking, and rapid heartbeat can be eased with acupuncture and TCM.
Claustrophobia is actually quite common; at least 10% of people report experiencing some claustrophobic feelings. Women report having a fear of confined spaces more often than men do. Phobias are sometimes rooted in a childhood experience, but they can arise in anyone, at any age, and are considered mental health issues or psychiatric disorders.
Phobias are distinct from regular fears because of their intensity and, to some extent, irrational nature. Phobias are unreasonable fears; feeling very afraid, to the point of physical and emotional distress, of something that isn’t really happening. Claustrophobia becomes a serious mental health problem if it interferes with a person’s daily life or relationships.
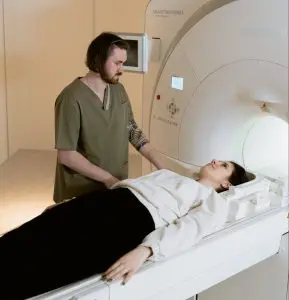
Sometimes claustrophobia can get in the way of a person getting help for other health problems. For example, it may cause them to avoid undergoing an MRI. Some people might fear visiting a doctor’s office, which often means facing elevators, public restrooms, and other small rooms without windows. Some women report feeling claustrophobic during pregnancy, as if they are “trapped” inside their own bodies.
Other common triggers of claustrophobia include: airplanes, trains, tunnels, small cars, revolving doors, or amusement park rides with restraints. Even thoughts of having to be trapped in one of these situations can be enough to bring on symptoms of claustrophobia. Signs of claustrophobia can be similar to those of a panic attack.
Top 10 Symptoms of Claustrophobia:
- Sweating
- Shaking or trembling
- Trouble breathing
- Rapid heartbeat, fast heart rate, high blood pressure
- Tight feeling in chest, chest pain
- Flushed face, feeling hot
- Dizziness, feeling lightheaded or faint
- Ringing in ears, tinnitus
- Butterflies in stomach feeling, nausea, queasy feeling
- Numbness or tingling in parts of the body
Other signs of anxiety due to claustrophobia could include: dry mouth, difficulty swallowing, choking, chills, confusion, or disorientation. In addition to physical symptoms of panic, claustrophobia may cause a person to cry, yell, or to be overwhelmed by a desire to get out of a situation because they feel that they are in serious danger, even if it seems irrational.

Cleithrophobia is another type of anxiety disorder that is sometimes confused with claustrophobia. Cleithrophobia specifically refers to the fear of being trapped or confined with no way to escape. Claustrophobia is a fear of the small space itself. These two phobias can exist together. Either one could cause serious anticipatory anxiety, for example, if a person has to have an MRI.
Cleithrophobia is related to other “winter phobias,” which may include “cabin fever,” which is a sense that one is stuck inside, or a fear of being literally trapped in the ice or snow. Many people feel an extra sense of sadness or dread during the winter months; this kind of depression is known as SAD (seasonal affective disorder).
Over time, repeated panic attacks or bouts of intense anxiety brought on by claustrophobia can create long-term stress that is harmful to overall physical and mental health. Acupuncture and TCM offer an adjunct or alternative treatment for claustrophobia which can help reduce symptoms and offset the effects of stress.
What Causes Claustrophobia?
Phobias can be triggered by some event or experience in which a person felt endangered and was traumatized, similar to PTSD (post-traumatic stress disorder). Like other mental health conditions, claustrophobia is influenced by brain chemistry. Imbalances in the neurotransmitters in the brain can cause some people to experience symptoms of anxiety or panic attacks even if nothing scary is really happening. Then, they may associate those physical and emotional feelings with a specific place or situation, which causes the anxiety to be triggered whenever they approach that place or even think of that situation.
People can perceive things differently. One research study suggested that people with claustrophobia may have a different perception of how near something, like a wall, is to them. In other words, they underestimate distances, or their sense of “personal space” is different from other people’s.
The amygdala is the part of the brain that processes incoming sensory information from the environment and signals the autonomous nervous system if it detects danger. This is essentially the neurological pathway of fear. Some research has suggested that people who experience panic disorders are more likely to have a smaller-than-average amygdala.
Treatment for Claustrophobia
To be diagnosed with claustrophobia, a person will need to explain to their doctor that they have been having these intense feelings for a while and that they are having a negative impact on their lives. This could mean that they go out of their way to avoid certain places or situations. A mental health professional will try to determine whether these fears are normal, or could be attributed to some other condition.
Some doctors may prescribe SSRIs like Zoloft or Lexapro, which influence serotonin levels in the brain, to help patients who are suffering from claustrophobia or anxiety. Often therapy is recommended to help patients learn to cope with their feelings. Cognitive behavioral therapy (CBT) and/or exposure therapy aim to retrain the mind and may help people learn to get used to being in a small space without feeling so anxious.
Psychiatric medications can have unwanted side effects and may create a sense of dependence. Some people will avoid therapy because it can be very confronting and become another source of fear.
Acupuncture and other TCM modalities, including herbs and movement techniques like Tai Chi, may offer an alternative solution for panic attacks due to claustrophobia, without side effects or having to work through the problem with uncomfortable talk therapy sessions.
Can Acupuncture Help Claustrophobia?
According to TCM, the organ systems closely associated with fear are those of the kidneys, liver, and heart. Kidney deficiency, in particular, can cause fear and mental disturbances. These types of mental disorders can also be related to imbalances in Yin and Yang energies, and blood deficiencies. An acupuncture practitioner’s approach to treatment for claustrophobia may, therefore, focus on strengthening and nourishing the kidneys, while soothing the liver and heart.
One study compared patients who knew they had claustrophobic feelings going into an MRI; some were treated with acupuncture based on TCM acupoints. Control groups patients were given sham acupuncture (not really the points that would correspond with TCM theory). They concluded that the real acupuncture treatment did offer a therapeutic effect for claustrophobia, with a 92% rate of effectiveness; meaning, the patients were able to remain calm during the MRI.
A case study of a woman who had experienced bouts of claustrophobic symptoms since her teenage years, including shortness of breath, trembling, sweating, and loss of motor control in her hands and feet. After six acupuncture treatment sessions, she reported much improvement: feeling calmer, no headaches, palpitations, or anxiety. Chinese herbs can also be used, in conjunction with acupuncture treatment, help a person overcome claustrophobia.
Acupressure Points for Claustrophobia
In between acupuncture sessions, you can use self-care acupressure to relieve claustrophobia.
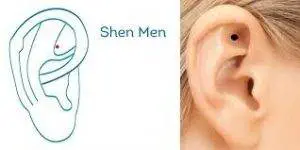
Shen Men is a Master point, located in the valley of the upper part of the ear. This is a classic point to help feelings of anxiety.
Shoujie, which is located on the palm of the hand between the metacarpals of the fourth and fifth fingers, along the topmost crease, helps relieve palpitations and dizziness.
Acupuncture for Claustrophobia Near Me in Los Angeles Area
TCM is an excellent way for people to find relief from mental health issues of all kinds, including depression, anxiety, panic attacks, and phobias. We will do all we can to make sure that you are comfortable in one of our larger treatment rooms with a window, and to make your acupuncture treatment experience relaxing and pain-free. If you or someone you know is finding that the thought of enclosed spaces is creating anxiety in day-to-day life, please do not hesitate to try acupuncture for claustrophobia.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.
How to Improve Mental Health With Acupuncture and TCM
By Xiaomei Cai, L.Ac., Ph.D. & Qineng Tan, L.Ac., Ph.D.

Mental health problems are becoming more and more prevalent, yet more than half of Americans experiencing mental illness do not get treatment. Mental disorders like depression, anxiety, panic attacks, PTSD, SAD (seasonal affective disorder), OCD, and postpartum depression can be improved with acupuncture and TCM, without negative side effects.
According to the most recent statistics, 19% of all adults in America are currently living with mental illness, while 15% of teenagers report having experienced major depression. Anxiety is the most common mental health condition, with 18% of the population reporting some form of anxiety disorder every year.
Addiction and substance abuse are also on the rise among both adults and teens. About 20% of people who have a mental disorder also have a problem with drug or alcohol addiction. Many people use drugs and alcohol to mask symptoms of depression and anxiety, but this only compounds the problem.
Mental health is about our emotions, our thoughts, and our relationships and social interactions with others. Mental health issues affect our behaviors, our thought patterns, and our responses to stress. TCM is an excellent form of care for mental health, because we take the whole person and their symptoms–mental, emotional, and physical–into consideration every time we work with them.
It is generally understood that mental health problems can come about due to a combination of factors, including imbalances in brain chemistry, trauma or abuse, and genetics or family history of psychological disorders.
Typical treatment for depression, anxiety, and other mental health problems involves talk therapy and/or prescription medications like antidepressants. Many people are not getting the relief they need from these forms of therapy, and medications can cause unwanted side effects, including headaches, nausea, weight gain, and trouble sleeping.
TCM takes a holistic approach to mental health and can help relieve signs of depression and anxiousness. TCM herbs and acupuncture can also provide an alternative treatment for many chronic illnesses that can contribute to depression.
Who Is At Risk for Depression, Anxiety, and Other Mental Disorders?

Everyone feels deep sadness and worry at times. When these feelings persist for a long time, they need to be addressed. Anyone, at any age, can experience symptoms of anxiety or depression. But some people are more at risk for mental health problems.
Risk Factors for mental illness include:
- Family history – if other people in your family have experienced mental illness, you may be more likely to have mental health issues, too.
- Stress – people who are going through financial insecurity, severe job stress, the loss of a loved one, or the breakup of a relationship are more likely to feel depressed.
- Trauma – having gone through a traumatic experience, such as abuse in a relationship, or being in an accident, or witnessing something terrible, can lead to feelings of depression, anxiety, or PTSD.
- Minority and marginalized communities – people who have experienced discrimination due to their race/ethnicity, gender, or sexual orientation are at a higher risk for mental health problems and often face extra barriers when they try to get help.
- Head trauma – having an injury to the head or brain can cause mental disorders.
- Chronic illness – having a longstanding serious illness or pain condition that dramatically impacts a person’s quality of life can lead to depression.
Medical science has been able to discern that certain imbalances in brain chemistry, including malfunctioning neurotransmitters in the brain and nervous system, are part of the physical root cause of depression, anxiety, and other mental disorders. Low serotonin, especially, is associated with a depressed mood, insomnia, panic attacks, obsessive-compulsive disorder (OCD), and even suicidal ideation. This is why the medical solution for depression and anxiety is often prescription medications like SSRIs, which impact the levels of serotonin in the brain.
Acupuncture and other TCM treatments can also have a positive effect on neurochemistry, without the dependence or side effects that medications can cause.
Can Acupuncture Help Mental Health Problems?
TCM has become more and more accepted by the scientific community as an effective way to relieve depression, anxiety, PTSD, and other mental disorders.
The Five Elements Theory used in TCM allows us to link physical, emotional, and mental symptoms of depression and anxiety and see specific patterns.
A medical doctor or therapist may hear that a patient has headaches, gastric upset, sleep problems, and episodes of anger, and view these as separate symptoms, treatable by separate medications. The acupuncturist sees a pattern that points to a particular imbalance in the organ systems.
TCM can help many mental health issues, including:
- Depression – according to TCM, depressed mood is usually related to some form of stagnation in the Qi of the liver, kidney, spleen, and/or heart. Feelings of grief are associated with the lungs.
- Anxiety – Depression with anxiety is often due to a deficiency of Yin, which can cause sleep problems, back pain, and irritability. Excessive worrying is related to the spleen. Studies have indicated that acupuncture treatment facilitates the release of serotonin, endorphins, and norepinephrine, which can help to calm feelings of anxiety, even immediately after treatment.
- Panic Attacks – TCM can help people with panic disorders. The intense feelings of fear that can come on with a panic attack may be related to the kidneys, which are involved in the release of adrenaline and cortisol, the “fight or flight” hormones.
- PTSD – Sometimes people suffering from PTSD or other trauma-related mental health problems are unable to go through talk therapy in order to deal with their feelings. There can be all kinds of reasons why a person is not able to speak about abuse or horrors they have suffered. Acupuncture treatments offer a real solution to ease the heavy feelings. A TCM provider offers healing by being able to sense a person’s energy, and facilitate shifts in that energy.
- SAD – Some forms of depression are temporary, but that doesn’t mean that they aren’t serious or don’t require attention. Seasonal affective disorder (SAD) affects many people, year after year. Acupuncture can help prevent this cycle from recurring.
- PMS/PMDD – People who menstruate often experience PMS (premenstrual syndrome), which can have emotional and mental symptoms. PMDD, an extreme form of PMS, can cause severe feelings of depression and even suicidal ideation. Acupuncture and herbs are an excellent way to address all kinds of problems with the menstrual cycle, including intense mood swings.
- Postpartum Depression – Many women experience depression during pregnancy and postpartum depression after having given birth. This condition, brought on by dramatic changes in hormones, can affect a new parent’s ability to care for themselves and their baby. Acupuncture treatment can effectively address postpartum depression, without fear of side effects from drugs.
- ADD/ADHD – ADD/ADHD are mental health disorders that affect a person’s ability to concentrate and can cause hyperactivity, mood swings, and social problems. Acupuncture and TCM can help both adults and children who are having problems with attentiveness, frustration, and restlessness.

Acupuncture can also help people who are struggling with substance abuse and addiction. Addictive behaviors are related to brain chemistry, and acupuncture can be utilized as an effective treatment for symptoms of withdrawal and as support for the mental and emotional aspects of recovery from alcohol or drug addiction.
Many people who are living with serious chronic illnesses also suffer from depression. When a health condition impacts a person’s quality of life every day, it can feel defeating and exhausting.
Neurological disorders that affect the brain, such as Alzheimer’s, dementia, and Parkinson’s disease, can create feelings of anger and frustration, bringing about changes in personality.
Autoimmune disorders like Crohn’s disease, Rheumatoid arthritis, ME/CFS (chronic fatigue syndrome), Lyme disease, MS (multiple sclerosis), and Lupus–can also engender feelings of depression because it can be so difficult to find treatment for their symptoms. People with serious conditions like HIV/AIDS and ALS are also apt to suffer from depression. Acupuncture and TCM not only provide help for the depression, but may be able to provide an adjunct or alternative treatment for these conditions, providing long-sought relief from symptoms and frustration.
Acupuncture Near Me For Mental Health Care in Los Angeles
If you or someone you know is suffering from mental illness, consider acupuncture as an alternative or adjunct to therapy and medications. People with mental health issues need a support system. At Art of Wellness in West LA, we have over 30 years of experience helping people find relief from the emotional, mental, and physical symptoms of anxiety and depression.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.