-
 Art of Wellness Acupuncture & Traditional Chinese Medicine (TCM)11704 Wilshire Blvd, Suite 295, Los Angeles, CA, 90025
Art of Wellness Acupuncture & Traditional Chinese Medicine (TCM)11704 Wilshire Blvd, Suite 295, Los Angeles, CA, 90025
myartofwellness@gmail.com310-451-5522 Office Hours
MonClosedTue7:30 am --4 pmWed7:30 am --4 pmThu7:30 am -- 4 pmFri7:30 am -- 4 pmSat7:30 am -- 4 pmSunClosedOur office opens from Tuesdays to Saturdays 7:30 am to 4 pm, will be closed on Memorial day, Independent day, Labor day, Thanksgiving day, Christmas and New year.
-
Recent Posts
- How to Treat Thoracic Outlet Syndrome With Acupuncture and TCM
- How to Treat Dupuytren’s Contracture With Acupuncture and TCM
- How to Treat Nutcracker Syndrome With Acupuncture and TCM
- How to Treat Rosacea With Acupuncture and TCM
- How to Treat Perioral Dermatitis With Acupuncture and TCM
- Lymphatic Drainage With Acupuncture and TCM
- How to Treat Turf Toe With Acupuncture
- How to Treat Nerve Pain With Acupuncture and TCM
- How to Treat Watery Eyes With Acupuncture and TCM
- How to Treat Ovarian Cysts With Acupuncture and TCM
- How to Treat Dystonia With Acupuncture and TCM
- Can Acupuncture Help Bad Breath?
- How to Treat Atopy with Acupuncture and TCM
- Plantar Fasciosis Treatment With Acupuncture and TCM
- How to Protect Yourself When Air Quality Is Poor
- How to Treat Spinal Headache With Acupuncture and TCM
- Sign up to receive news and updates and get my free report:“The Top 10 Reasons to Try Acupuncture”

August 2025 M T W T F S S 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31
Insomnia
The Ultimate Guide to the Acupuncture Point on Head for Headaches
by Xiaomei Cai, L.Ac., Ph.D. & Qineng Tan, L.Ac., Ph.D.
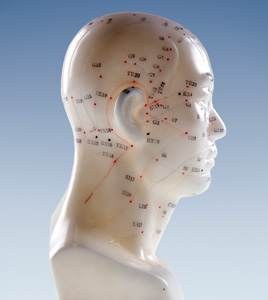
Why does the TCM doctor always put an acupuncture needle in top of head? If you’ve had acupuncture before, it’s likely that your acupuncturist used some acupuncture points on head during your treatments. Using pressure points on the head is something TCM doctors do often, because there are so many useful acupressure points on the head, especially acupuncture points top of head. There are head pressure points for headaches, points to relieve migraines, acupressure head points to help anxiety, fatigue, allergies, and many other conditions.
Even if you’re coming in for acupuncture to help some other condition, whether it’s chronic pain, an autoimmune disease, heart problems, or kidney problems, probably at some point your acupuncture practitioner is going to use acupoints on head to help you relax during your treatment. Every single person who comes into our office for acupuncture is suffering from some form of stress, and using certain points on the top of the head can help with stress relief right away.
Other common reasons to use pressure points in neck and head include:
- to fight fatigue
- headache and migraine
- allergies, asthma, hives, rhinitis, sinus problems, common cold
- anxiety
- nervous disorders
- thyroid disorders
- hormone imbalances
- more mental focus, improved memory and cognition
- tinnitus, ringing in the ears
- vertigo, Meniere’s disease
- toothache, dental pain, dental anxiety
Why are pressure points on the head so powerful? To answer this question, let us explain a bit about the meridian system in TCM.
TCM Meridian Head Points
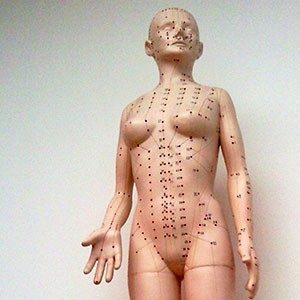
TCM is based on interdependent systems of organs and energy channels that run through the body. The channels are known as meridians, and along them flows Qi, the life energy that animates the body and all of its functions. There are 12 major meridians and 8 major vessels; the meridians are close to the surface of the skin, and the vessels, which essentially connect all the meridians, are deeper inside the body. While the way in which we think of the meridian pathways is more metaphorical than physical in nature, they can be considered roughly analogous to the circulatory system of blood vessels or the network of nerves of the nervous system as we think of them in conventional Western medicine.
Along the meridians lie acupoints, specific points that we stimulate with acupuncture needles during acupuncture treatment or with the fingers and thumbs during acupressure massage. The interconnectedness of the organs, meridians, and individual points is the foundation of acupuncture theory.
We use specific points on a meridian in order to address issues in a particular organ or organ system that corresponds (energetically) with that meridian. There are several pressure points for head and neck pain, points to help relieve allergies, pressure points for frontal headache, and more.
Several of the major meridians originate or end in the head:
- Gall Bladder (GB) meridian – points of the gall bladder meridian wrap around the side of the head, the forehead above the eyebrow, the temple, around the ear, and down the back side of the neck–just as the pain of a migraine often does. Then it continues down from the intersection of the neck and shoulder, zig-zagging across the torso, and finally running down the leg and ending in the fourth toe. This meridian is used to treat severe headaches, stress, tension that affects the shoulder and neck, and bile-related problems.
- Large Intestine (LI) meridian – begins at the points of the index finger, travels up the arm, through the shoulder and neck, then comes up to the lower corner of the nose. This meridian is involved in “letting go,” both from the eliminatory organs of the lower body, and exhalations from the nose.
- Stomach (ST) meridian – the ST meridian starts near the eye, swoops up to the side of the top of the head, comes down next to the mouth, and continues down through the neck, chest, center of the body, down the leg, ending at the point of the second toe. This meridian is used to treat Shen (spirit) disorders, like insomnia, anxiety, palpitations, memory problems, and blood deficiency.
- Small intestine (SI) meridian – originates in the little finger, runs up the arm into the shoulder and then branches out, some of it going into the major organs of the heart, stomach, and small intestine; then other branches go up into the face, by the cheekbone and right in front of the center of the ear. The SI is used to treat fevers and mental health conditions, among other things.
- Bladder (UB) Meridian – begins at the inner canthus of the eyes, goes up and over the top of the head, about an inch away from the midline on either side, and then all the way down the back and leg, ending in the little toe. Used to help with invasion disorders (wind, cold, heat etc.) that affect the eyes, sinus headaches, allergies, stuffy head, neck pain and stiffness.
- Triple burner meridian, also known as San Jiao (SJ) – begins at the tip of the ring finger, then goes up the arm, through the shoulder and chest, up the side of the neck and comes up around the ear, and into the temple and outer brow bone. The San Jiao head points are used to work on dizziness, headaches, eye twitching, and dental pain.
- Conception vessel – also known as the Functional Channel, or the Front Channel, or Ren Mai, this vessel originates at the navel, then drops down to the perineal area, and runs back up the center of the front of the body, ending in a point on the chin, in the dip just under the lower lip. This vessel controls the Yin energy of the body and is essential to the health of the reproductive organs and fertility.
- Governing vessel, also known as the Extraordinary vessel, the “Sea of Yang” or Du Mai – originates in the lower back near the kidneys, runs up the spine and around and over the top of the head, ending in the middle of the face. This vessel controls the Yang energy of the body, and in particular the kidneys, the back and spine.
Top 10 Acupuncture Points on Head

Of course, your acupuncturist will not only use acupoints on your head during a treatment session. We choose a variety of points that will work together to alleviate symptoms and help optimize the functioning of the organs. These specific head points may be used as part of a treatment to work on a specific symptom or condition:
- Yin Tang, or the “Hall of Impression” – this is what is called an “extraordinary point,” meaning it doesn’t really belong to a meridian; it stands on its own. Right in the third eye, it is used to reduce anxiety, vertigo (dizziness), help promote better sleep, clear wind and congestion, and relieve sinus pain and headache.
- DU21 – Shen Ting, “Spirit Court” – Right in the front middle of the top of the head, about an inch above the hairline. This is one of the pressure points for frontal headache, also good for sinusitis, nosebleeds, anxiety, panic attacks, and sleep problems.
- DU 20 – Baihui, or “The meeting of the 100s” – right in the very center of the top of the head, master of endocrine and nervous system, used for anxiety, fatigue, mental focus, relaxation, hypothyroid, adrenal problems, hormone imbalance, headaches.
- Si Shen Chong – “Four Alert Spirit” – this is actually a set of four “extraordinary points,” which surround DU20. Very helpful for sleep disorders, memory disorders, dizziness, and headaches.
- GB20 – Feng Chi, “Wind Pool,” low back of the head, where the skull meets the neck muscles, helps headaches, migraine, blurred vision, fatigue, neck pain and stiffness. We may use this point when a patient has a cold; this is a point where cold wind can get into the body, and why it is important to wear a scarf to protect your neck when it’s cold and windy out.
- Taiyang “Great Sun” – Right in the depression of the temple, this point can help dizziness, one-sided headaches, migraines, sensitivity to light, and jaw pain, TMJ.
- GV26 Shui Gou – in the mustache area, between the nose and mouth, right in the center of the crease, this point helps to calm the mind and restore mental focus. Also used as first aid when a person faints or is in shock. Helps stop hiccups. Helps with serious neurological disorders like epilepsy, seizures. Also good for low back strain.
- LI20 Ying Xiang “Welcome Fragrance” – located in the lower corner of the nose, right in the nasolabial groove, used to alleviate congestion, allergy itching in the nose, and to clear the nasal passages.
- ST8 – Touwei, about 5 finger widths above the eyebrow, dispels dampness, used for “splitting headaches,” frontal headache, migraines, headache with nausea and/or vomiting, vision problems, tearing eyes, eye twitching, dizziness/vertigo, hair loss. Helps with mental health, when a person is “overthinking” things, or having repetitive thoughts.
- BL2 – Zhanzhu – located at the inner corner of the eyebrow, good for itchy, watery eyes due to allergies, other eyes problems like glaucoma, night blindness, and sinus headache.
Facial Acupuncture Points

As we have mentioned, some pressure points on the face are used to help relieve sinus congestion, nasal congestion, and other issues related to common colds and flus or allergies. Points on the face may also be used to help the facial paralysis of Bell’s Palsy, or TMJ jaw pain.
Naturally, we also use acupuncture points on the face as acupuncture points for the face, that is, when we are striving for facial rejuvenation. This technique is sometimes called an acupuncture facial. Using points on the face can help to stimulate collagen production, help to tighten the skin, reduce the appearance of wrinkles, and strengthen the facial muscles. People of all ages and genders can benefit from acupuncture skin care. Cosmetic acupuncture can treat signs of aging skin like sagging, puffiness under the eyes, and dryness.
Self-Care With Acupressure Head Points

What is acupressure? Acupressure is a form of massage that goes back thousands of years in Chinese Medicine. Stimulating the same points we needle in acupuncture treatment with your fingers and thumbs can be beneficial for different types of headaches and neck stiffness, to calm anxiety, and bring more mental clarity.
Choose a time when your environment is quiet and free of distractions, the same as you would for a meditation practice or home workout. Be sure to breathe deeply and smoothly as you perform self-acupressure. Press firmly, applying deep pressure to a point in a small, gentle circular motion. Giving yourself an acupressure treatment only takes a few minutes, and it is a great way to take care of yourself between acupuncture sessions.
Acupuncture Near Me for Headaches and More
Every time you come in for acupuncture treatment, your TCM doctor is looking for ways to treat your overall condition, but also focusing on how you are feeling right now, today. Often, people are feeling tired and stressed, beyond and in addition to the health condition that caused them to seek out alternative medicine in the first place. Using points on the head that help fatigue, calm a racing mind, and reduce the physical effects of stress is one way that your acupuncturist is practicing preventative care, while at the same time, making sure you leave your treatment feeling rested and reenergized. The next time you come in for a visit, be sure to let us know how you’re feeling, and feel free to ask us, “What is that point on my head for?”
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.
How to Stop Snoring With Acupuncture and TCM
By Qineng Tan, L.Ac., Ph.D. & Xiaomei Cai, L.Ac., Ph.D.

Have you been told you’re snoring loudly? Do you feel tired even after 8 hours of sleep? Waking up with a dry mouth, feeling tired all the time, and having trouble staying asleep at night are all signs that you might have sleep apnea. Sleep apnea is a sleeping disorder in which normal breathing is interrupted repeatedly. Acupuncture and TCM offer a natural way to treat obstructive sleep apnea, insomnia, fatigue, and other sleep-related problems.
Sleep Apnea (also known as sleep apnoea) is when a person does not breathe normally during sleep. When there is a pause in normal breathing during the night, the body is not getting enough oxygen, and the brain sends an urgent message to start breathing again. The person wakes, so briefly that they usually do not remember it, gasps for air and starts breathing again. Often people do not realize that they are snoring or making snorting or choking sounds while they sleep unless another person tells them it’s happening. Because of this, many cases of sleep apnea go undiagnosed, and people go on feeling fatigued all the time.
While people of any age or gender can experience sleep apnea, it is most common among older men. There are a few different kinds of sleep apnea; the most prevalent type is obstructive sleep apnea (OSA), in which the throat and/or airway is physically obstructed by the positioning of the neck, jaw, and soft tissues of the throat, like the tongue and uvula. OSA is associated with being overweight or obese, because extra weight can affect the musculature of the upper respiratory system. Women who have already gone through menopause are more likely to develop sleep apnea because postmenopausal weight gain is more likely to occur in the upper body than it does prior to menopause. Sleep problems and obesity are related in many ways; getting less sleep or poor quality sleep can cause people to gain weight or have trouble losing weight. People with diabetes and/or metabolic syndrome are also at higher risk for obstructive sleep apnea.
Besides disturbing sleep and causing fatigue, apnea can lead to other serious health conditions, especially cardiovascular problems like high blood pressure, irregular heartbeat, and stroke. Sleep apnea can increase the heart rate and the production of stress hormones. Men with OSA are more likely to experience erectile dysfunction (ED). Lack of quality sleep can also have a negative impact on mental health, contributing to depression, anxiety, and cognitive decline.
The typical treatment for snoring involves the use of a sleep apnea machine, called a CPAP machine (continuous positive air pressure machine), which pushes air into the nose while you sleep, ensuring that the airway stays open and continuously active. This treatment can help people breathe easier throughout the night, but some people may find the machine noisy and uncomfortable.
TCM methods like acupuncture treatment for snoring and sleep apnea offer a way to address these problems at their source holistically, helping people to sleep well and breathe more freely.
Top 3 Types of Sleep Apnea
Sleep apnea causes loss of oxygen due to shallow breathing (hypopnea) and/or interrupted breathing while sleeping. Different types of sleep apnea are classified by their physiological causes:
- Obstructive sleep apnea (OSA) – this is caused by the improper relaxation of the throat muscles while sleeping.
- Central sleep apnea (CSA) – is caused by disordered signalling from the brain to the organs that control breathing.
- Complex sleep apnea – (or treatment emergent sleep apnea) is a combination of both of the above.
Restless legs syndrome (RLS), also known as Willis-Ekbom disease, is a condition wherein a person has an uncontrollable urge to move the legs, or sometimes arms or other parts of the body, accompanied by a sensation of itching, burning, crawling or throbbing. This usually happens when the person is lying in bed, trying to fall asleep. Restless leg syndrome can coexist with OSA, compounding the problem by making it difficult to get to sleep or stay asleep during the night.
Narcolepsy is a sleeping disorder in which overwhelming sleepiness during the daytime causes people to suddenly and uncontrollably fall asleep. Many people who suffer from narcolepsy also have sleep apnea. In this case, the sleep problem is not related to breathing so much as how the brain and body are moving through sleep cycles, like REM sleep. For people who have narcolepsy, treatment with a CPAP machine is often not very helpful.
Sleep apnea or snoring does not seem to be related to other abnormal sleeping behaviors (parasomnia), such as sleepwalking, night terrors, or sleep-related eating.
Top 10 Symptoms of Sleep Apnea

Many people snore and do not realize it. It is important to pay attention to the subtler sleep apnea symptoms. Signs of sleep apnea include:
- Loud snoring
- Interrupted breathing – moments during the night when the person’s breathing actually stops and then starts again
- Gasping for air while sleeping
- Waking up with a dry mouth or sore throat
- Headaches in the morning
- Insomnia, difficulty getting to sleep or staying asleep during the night
- Feeling very sleepy during the daytime (hypersomnia)
- Difficulty paying attention
- Feeling irritable
- Getting up often during the night to urinate (nocturia)
What Causes Snoring?

Sleep apnea is caused either by a physical obstruction of the throat and airways or by problems with brain signals to the breathing apparatus. Not everyone who has sleep apnea snores loudly. On the other hand, not everyone who snores necessarily has sleep apnea. Other reasons people snore may include:
- Congestion of the nose due to a cold or allergies
- In late pregnancy, the growing belly puts upward pressure on the respiratory system
- Sleeping pills, medications that work as relaxants, like Ativan or Valium
- Alcohol consumption
- Anatomy – large tongue or uvula, or swollen tonsils
People with sleep apnea are often advised to sleep on their side rather than on their back, as this helps prevent the obstruction, but it can be difficult for people to control their behavior while sleeping.
Treatment for Sleep Apnea

To firmly establish whether a person has sleep apnea, and what type, doctors will often evaluate the situation in a sleep study session. People will spend the night in a sleep center, where their heart and breathing functions are monitored (polysomnography).
CPAP machines are generally considered to be the best care available for sleep apnea. These devices can help stop snoring, allow a person to get more restful sleep, and cut the risks of serious issues like heart disease that are associated with sleep apnea. However, the machine does not actually do anything to improve the weak musculature that causes OSA or the disordered signalling that causes CSA. It is possible to swallow air while breathing with the CPAP machine, which can lead to gas and a bloated stomach. Some people may find the face mask, which must be strapped to the face, uncomfortable. The noise of the machine may be disturbing to the person using it, as well as to the person’s bed partner. It may be difficult for some patients to get used to using the machine, and if they are not using it regularly, they are not getting the health benefits.
There are also some oral appliances available, such as mandibular advancement devices (MAD), which are worn in the mouth to alter the placement of the jaw and tongue in order to keep the airway open during sleep. These can also be effective in terms of helping people breathe better while they sleep. Compared to CPAP, they are quiet, discreet, and cost-effective. Again, the main question is whether a person will be able to tolerate the device; some people may experience toothache or dental pain, TMJ jaw pain, dry mouth, or too much saliva.
Surgery for snoring and sleep apnea is usually only recommended if other methods of treatment have failed. Different procedures involve removing soft tissues (uvula, tonsils, adenoids), or changing the shape of the jaw bones. Small rods may be inserted into the upper palate to help keep the airway open. A device that monitors breathing and stimulates movement of the tongue may be implanted in the chest.
Sometimes people may use melatonin as a natural sleep aid. Melatonin may have a positive impact in terms of helping people fall asleep more easily. It also has strong antioxidant properties, which means it may help with the control of the breathing apparatus and the amount of oxidation a person is getting while sleeping. While it is generally considered safe as a health supplement, melatonin side effects can include problems with dizziness, headaches, and nausea, and it can also be contraindicated with other medications. Melatonin can affect blood coagulation, so it may be unsafe to take if a person is also taking blood thinners, for example.
Can Acupuncture Help Stop Snoring?
According to TCM theory, the spleen and stomach are responsible for transforming nutrients from food and fluids into Qi (life energy), which is then delivered to the heart and lungs. In the TCM view, sleep apnea is often a problem related to phlegm and Qi stagnation, as are many conditions related to fatigue or insomnia. If phlegm builds up and becomes stagnant in the spleen, the lungs cannot get the Qi they need. So, one possible differentiation for sleep apnea is Spleen Deficiency with Qi Stagnation. This condition of dampness and phlegm will often cause people to feel heavy and bloated.
In some cases, too much internal heat contributes to the problem. Snoring, combined with sweating, and waking up with a sore throat, is a sign that we need to clear heat and toxicity from the body.
Sleep disturbed by nightmares is associated with the gallbladder, while difficulty falling asleep is associated with the liver. An acupuncture practitioner will listen carefully to what specific symptoms of sleep apnea each individual patient is experiencing, and tailor the treatment accordingly.
A meta-analysis of over 200 randomized trials involving the use of acupuncture to treat sleep apnea concluded that acupuncture was more effective overall than CPAP treatment, in terms of improving breathing and oxygen levels.
Can Chinese herbs help snoring and sleep apnea? Specific herbs have been shown to help reduce inflammation and improve oxygen levels in patients with sleep apnea. Chinese herbal formulations can help stop snoring and reduce daytime fatigue.
Natural Remedies for Snoring

Acupressure can help snoring and sleep apnea. Since we are trying to clear heat and phlegm from the stomach, spleen, and large intestine, use acupressure points along the Stomach Meridian, which runs down the leg. On the front of the shin, apply pressure, kneading with your thumb, starting to the side of the shin bone a few inches below the knee, then moving down about 3 inches and doing the same thing. Knead each of the four points about 30 times as your move down the leg. If you are aware that one side of the nose is more blocked than the other while you are breathing during the night, practice the acupressure on the opposite leg. For example, if your left nostril is the one that is more stuffed up, do acupressure on the right leg.
Acupuncture Near Me for Snoring
As the population ages, and unfortunately, more people suffer from obesity and metabolic syndrome, sleep apnea is a growing health concern all over the world. Snoring can have a seriously negative impact on quality of life, health, and longevity. Conventional methods of treatment for sleep apnea can be effective, but many people find CPAP uncomfortable and inconvenient for long-term use. If you suspect you may have sleep apnea, or are worried because your partner snores loudly at night and seems to be gasping for air, do not wait to get help. Acupuncture and TCM herbs can help relieve fatigue due to snoring and reduce the risk of more serious problems related to sleep apnea.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.
How to Treat Musculoskeletal Pain With Acupuncture and TCM
By Qineng Tan, L.Ac., Ph.D. & Xiaomei Cai, L.Ac., Ph.D.

Do you experience unexplained pain all over the body? Muscle pain and tenderness, along with feeling tired all the time and having mood issues? Widespread musculoskeletal pain accompanied by fatigue or feeling exhausted may be a sign you have fibromyalgia. Alternative medicine methods like Acupuncture and TCM offer a way to help ease the chronic pain, sleep problems, and emotional disturbances caused by fibromyalgia.
Fibromyalgia (sometimes referred to as “fibro” or FM) is one of the most common chronic pain conditions worldwide, affecting an estimated 10 million people in the United States alone. Still, this chronic condition is still not well understood by medical science. There are no definitive tests to show whether or not fibromyalgia is the cause of pain all over the body along with chronic fatigue, so many people go on having musculoskeletal problems and hurting all over without being diagnosed or treated. There are many people who have fibromyalgia who also suffer from depression and anxiety related to the illness. Fibromyalgia can dramatically impact a person’s quality of life. While people of ages and genders can have fibromyalgia, it is much more prevalent among women.
Fibromyalgia is considered to be a syndrome: a collection of symptoms that often occur together. Fibromyalgia is associated with other conditions like lupus, rheumatoid arthritis (RA), myofascial pain syndrome, and myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). It may coexist with these other chronic conditions, or sometimes be mistaken for one of them. However, fibromyalgia is now understood by medical professionals to be its own distinct condition with specific manifestations.
People who have RA have been shown to have an increased risk for also having fibromyalgia. But the quality and location of the musculoskeletal pain differentiates the two conditions. The pain of fibromyalgia shows up in the musculoskeletal system in the areas where there are large muscles, causing pain that may move around throughout the torso, back, hips, thighs and arms. Fibromyalgia pain is often described as a kind of “tenderness,” or when the body aches all over. “Tender points” all over the body are specific to fibromyalgia. This is different from arthritis, which generally causes swelling and pain in the joints. Both RA and lupus are understood to be caused by inflammation, while fibromyalgia is believed to be caused by a problem with the central nervous system (CNS), in which pain signals are amplified, causing extreme sensitivity and pain, even when there is no seeming reason for that area of the body to feel pain.
Some of the fibromyalgia symptoms are very similar to those of myalgic encephalomyelitis (ME), which is also known as chronic fatigue (CFS). As with RA and lupus, the two conditions can overlap. The difference is that the overwhelming symptoms of ME/CFS are related to fatigue or post-exertional malaise (PEM), while the predominant symptom of fibromyalgia is widespread muscle pain and tenderness.
Fibromyalgia seems to show up in some people due to a traumatic or triggering event. There can then be a fibromyalgia flare up due to the presence of other triggers later.
Fortunately, acupuncture, herbs, and other forms of alternative medicine that fall under TCM can approach all of the different symptoms of fibromyalgia holistically. Acupuncture is widely accepted to be effective for helping musculoskeletal conditions of all kinds, as well as neurological problems, rheumatological conditions, sleep issues, and emotional and mental health disorders.
Top 10 Symptoms of Musculoskeletal Pain

As a syndrome, fibromyalgia may manifest as any combination of a few or several of a variety of symptoms. The most common symptoms of fibromyalgia include:
- Widespread musculoskeletal pain: pain, tenderness, and/or stiffness in the muscles all over the body that may come and go or migrate from one area to another
- Fatigue, exhaustion, extreme tiredness
- Emotional and/or mental issues: depression, anxiety, PTSD
- Sleep problems, insomnia
- Cognitive issues: difficulty concentrating, memory problems, “fibro fog”
- Headaches, migraines
- Neuropathy: tingling or numbness in the hands and/or feet
- TMJ, jaw pain
- Digestive problems: irritable bowel syndrome (IBS), abdominal pain, bloating
- Bladder pain, interstitial cystitis
Other more subtle signs of fibromyalgia can include: itching all over, a skin crawling sensation (like bugs crawling on skin), extra sensitivity to smells or temperature, a tendency to shiver, or dry eyes or eye pain.
Top 5 Causes Musculoskeletal Pain Flares
The symptoms of fibromyalgia tend to come and go. Some days a person might feel almost totally fine, then other days, the fibromyalgia flares, causing more pain, exhaustion, and sometimes other symptoms. What triggers a fibromyalgia flare up?
- Hormonal changes during menstrual cycle, miscarriage, pregnancy, or postpartum
- Prolonged stress
- A sudden traumatic event, PTSD trigger, panic attack
- Changes in weather: temperature, humidity, barometric pressure
- Lack of sleep
When one of the 18 tender points of fibromyalgia is touched, it can trigger more widespread pain. These points include areas like: the front and sides of the neck, the base of the skull, the elbow, and the backs of the knees.
What Is the Treatment for Fibromyalgia?
Medical treatment for fibromyalgia typically involves a combination of medicine to alleviate pain with psychological support and lifestyle management. Drugs like Lyrica, Cymbalta, and Savella are approved for prescription for patients with fibromyalgia. Lyrica and Cymbalta are also used to treat conditions that involve nerve damage or nerve pain, like diabetes, neuropathy, shingles, while Savella works in a way that is similar to antidepressants. Other pain relievers and/or antidepressant medications may also be prescribed to help people manage pain of fibromyalgia, help them sleep better, and boost mood. All of these medications can come with unwanted side effects, and they do not help to relieve pain in every case.
People with FM pain will often receive counseling on how to manage their condition by being very careful not to exert themselves or become exhausted. Getting quality sleep and reducing stress can help to prevent fibro flare up. It can be hard for people to follow guidelines that ask them to make major lifestyle changes. Fortunately, acupuncture, herbs, and the patient support of a TCM practitioner can offer more help for people with fibromyalgia.
Acupuncture for Musculoskeletal Pain
Can acupuncture help fibromyalgia? Yes. TCM offers a comprehensive system for managing musculoskeletal pain and chronic pain, helping to heal nerve damage and restore central nervous system function, supporting mental health, relieving anxiety and depression, and addressing sleep problems. Whereas with conventional medicine, a patient might go from one doctor to another to handle all of these issues, the acupuncturist can address them all at once. The TCM point of view always takes into consideration the connection between what is going on physically with what is going on emotionally in each individual, so it is really an excellent way to help patients with fibromyalgia.

Like Western medicine, TCM recognizes that sometimes fibromyalgia can be originally caused by a traumatic event or an extremely stressful time in one’s life. Emotional upheavals cause stress to the liver, which in turn causes stagnation of blood and Qi. TCM also sees coldness and dampness as pathogenic forces that can have a profound effect on overall health. According to TCM, widespread musculoskeletal pain falls under the category of Bi Syndrome. In Bi Syndromes, cold and damp get into the body and take hold on a deep level, causing pain and stiffness. With acupuncture treatment for fibromyalgia, we seek to clear cold and damp, and restore good flow of Qi and blood throughout the body.
Acupuncture has an analgesic effect, relieving muscle pain without side effects. Moxibustion may be utilized to bring warmth to areas of the body. Cupping is another modality used to draw out damp cold and improve blood flow. Tai Qi and Qi Gong, gentle therapeutic movement practices that have been developed over 1000s of years as part of TCM, also may offer great benefits for people with FM.
A systematic review of over 400 studies of fibromyalgia treatment with TCM, acupuncture treatment was found to be effective for reducing both short term pain and long term pain.
Another review found that acupuncture and herbs worked better to reduce pain than standard medication therapy.
Top 5 Tips for Managing Fibromyalgia

Dealing with fibromyalgia and seeing significant improvement in fibro pain will probably involve making some lasting lifestyle changes. Making adjustments to your sleep habits, food choices, and your exercise routine can make a difference in preventing the next FM flare up.
- Choose a gentle, enjoyable form of exercise. Start slowly, and gradually increase the amount you can exercise over time. Walking outdoors is a great option, as are Tai Qi and Qi Gong.
- Limit or eliminate caffeine and alcohol. These substances can interfere with getting good sleep and exacerbate liver problems. Alcohol is not safe to consume if you are taking medications for fibromyalgia like Lyrica, Cymbalta, and Savella.
- Avoid sugar, which may give you a short-lived good feeling, but will lead to a “sugar crash,” and feeling more exhausted than before. Any kind of simple carbohydrates, like foods made of white flour, or bottled fruit juices, can cause highs and lows in blood sugar. Avoid sugar substitutes and food additives like MSG, which can trigger reactions in some people.
- Focus on eating complex carbohydrates, especially vegetables. These help you have a more sustained energy throughout the day. Nuts and seeds are also good.
- Warm baths with Epsom salts can be very soothing.
Getting enough sleep at night, and even resting or napping during the day, may be essential to your well-being if you have fibromyalgia. Develop habits that allow for plenty of rest and set yourself up for a good night’s sleep.
Acupuncture Near Me for Musculoskeletal Pain
Many people who have fibromyalgia choose to try alternative medicine as a way of managing FM pain. Physiological conditions that stem from emotional stress are often not resolved through the use of medications. Acupuncture and TCM have a long history of helping people to heal from emotional disturbances that cause physical pain. Acupuncture treatment works to increase the flow of energy through the body and improve the connections between the brain and nerve endings. If you or someone you know suffers with fibro, consider acupuncture as a way to find relief from musculoskeletal pain and constant fatigue.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.
How to Treat Irregular Heartbeat With Acupuncture and TCM

Does if feel like your heart “skips a beat,” or your heart is “fluttering?” Maybe you feel your heart beat is fast or slow, compared to your normal heart rate. Lots of things can cause your resting heart rate to be uneven. Acupuncture and TCM can be beneficial as both an adjunct or alternative to drug therapy for paroxysmal supraventricular tachycardia, paroxysmal atrial fibrillation, and other types of arrhythmia that cause heart palpitations or a fast heart rate.
The pulse rate is controlled by electrical impulses that originate in the sinus node, which is located in the right atrium, or upper chamber, of the heart. The feeling that your heart rhythm is off, or different from your normal pulse rate is called Arrhythmia. The average resting heart rate is 60 to 100 beats per minute. A fast heart rate–more than 100 beats per minute–is called tachycardia. A slow heart rate–less than 60 beats per minute– is called bradycardia.
It is natural to have a slightly high heart rate during or just after exercise, or or a slow heart rate during sleep or times of relaxation, as when meditating. In some cases, a rapid heartbeat is related to anxiety or panic attacks. Sometimes a rapid or irregular heart rate may be related to caffeine consumption or a side effect of some medication. Other times, it may be a sign of heart disease or other chronic condition that needs to be addressed. Other symptoms related to irregular heartbeat include: shortness of breath, chest pain, sweating, and dizziness.
The heart is composed of four chambers; the top two chambers are called the atria, into which blood is received, and the two bottom chambers, the ventricles, from which blood is pumped out to the lungs and the rest of the body. Medical science classifies deviations from a normal resting heart rate both according to their rapidity and the chamber of the heart that seems to be problematic.
There are different medications available to help restore the regular rhythm of the heart, as well as therapies that deliver electrical impulses to the heart through a catheter, and devices, such as pacemakers or defibrillators.
In many cases, arrhythmia is not a serious problem. But in other cases, it can increase the risk of blood clots, stroke, and other life-threatening conditions. It is advisable to consult a medical professional if you are having an irregular heartbeat often enough to be concerned.
Acupuncture and TCM offer a natural way to help restore heart function and a good resting heart rate without the unwanted side effects of medications or invasive procedures.
Top 10 Types of Irregular Heartbeat

There are many different terms that describe deviations from a regular, healthy heart rate. Some irregular heartbeat issues are due to congenital conditions, while others may occur due to trauma, disease, or aging.
- Atrial flutter – an accelerated heart rate that occurs in an organized and rhythmic way due to rapid electric impulses in the atria.
- Atrial fibrillation (AFib or AF) – a rapid heart rate, also caused by increased electrical impulses in the atria that happen in a chaotic, arrhythmic way. Fibrillation refers to the rapid and irregular movement of muscles. In the case of AFib, the upper chambers of the heart quiver quickly. This condition is associated with stroke. AFib with RVR (rapid ventricular response) is a condition that occurs when patients are critically ill, often in the ICU, when the atrial fibrillation causes the ventricles to beat faster.
- Ventricular fibrillation – rapid impulses in the ventricles (the lower chambers of the heart) cause ineffective pumping of blood out to the body.
- Supraventricular tachycardia – this refers to types of arrhythmia that originate in the atria (above the ventricles) and cause brief episodes of accelerated heart rate.
- Ventricular tachycardia – a fast but regular heart rate that does not allow the ventricles to fill with as much blood as usual.
- Sick sinus syndrome – more common among older people, this is when the sinus node is malfunctioning and may sometimes cause a fast heart rate, and other times, a slow heart rate.
- Long QT Syndrome – a heart disorder found in people with a particular genetic mutation that causes rapid heartbeat and fainting spells.
- Wolff-Parkinson-White Syndrome – some people are born with an extra electrical pathway that can cause extra or irregular signalling to occur.
- Conduction Block – a block of the electrical pathways that sometimes results in a slower heart rate.
- Premature ventricular contractions – this is when an extra heartbeat beat originates from the ventricles, rather than the atria. It can feel like a “skipped” beat, or your heart pounding or jumping in your chest, but it is actually a kind of extra beat. This can happen occasionally due to drug stimulants like caffeine or nicotine, or other medications like decongestants or antihistamines. It can also be due to heart disease creating scarring in the ventricles or in the structural parts of the heart that hold the pathways for electrical impulses.
Atrial fibrillation increases the risk of blood clots and strokes because blood is not being effectively pushed from the atria into the ventricles, so blood pools or collects in the atria.
What Causes Irregular Heartbeat?
In general, most types of arrhythmia are caused by some disorder of the electrical conduction system that controls the beating of the heart valves, or weakness of the heart itself, which is known as cardiomyopathy.
Causes of tachycardia include:
- Not enough blood nourishing the muscles of the heart.
- Dilation or one or more valves of the heart, meaning that the muscle tissue becomes thinner and the chamber becomes enlarged.
- Thickening of the walls of the heart chamber makes them stiff; this is known as hypertrophic cardiomyopathy.
- Scar tissue makes the heart tissue more rigid (restrictive cardiomyopathy or dysplasia). This can happen due to inflammation, high levels of iron or protein in the tissues, sometimes as a side effect of cancer treatments (radiation and/or chemotherapy). Arrhythmic right ventricular dysplasia may be an inherited condition.
Causes of atrial fibrillation or atrial flutter include:
- High blood pressure
- damage to the heart from a heart attack or heart surgery
- Coronary artery disease
- Congenital heart defects
- Hyperthyroidism
- Lung disease, infections, or pneumonia
- Sleep apnea, snoring
- Smoking or overuse of other chemical stimulants
Chronic conditions like diabetes, obesity, metabolic syndrome, kidney problems, alcoholism, Parkinson’s disease, or a family history of heart problems increase a person’s risk for developing an arrhythmia.
Treatment for Irregular Heartbeat

There are several different types of medications to treat irregular heartbeat. Tachycardia may be treated with antiarrhythmic drugs, which work by suppressing or depressing the electrical impulses that are misfiring or transmitting signals too quickly. Beta blockers slow down the heart rate and reduce blood pressure by reducing the production of adrenaline. AFib treatment often involves anticoagulants or blood thinners, which prevent the formation of blood clots. In some cases, these medications can work to help people maintain a steady heart rate and prevent serious events like strokes. The downside is that they must be taken daily on an ongoing basis, and in some cases, they can actually cause the heartbeat to become even more erratic.
Medical procedures that are designed to help irregular heartbeat include: electrical cardioversion, in which an electric shock is used to help “reset” the heart rate, and ablation, in which the tissues that contain the electric impulse pathways are intentionally scarred in order to reduce their output. Implantable devices such as defibrillators or pacemaker monitor the heart rate and deliver small “shocks” to alter the rhythm of the heartbeat. For some people, these methods work to keep the heart functioning. In some cases, though, the surgery to implant the device causes complications or damage to critical tissues around the heart or lungs.
Can Acupuncture Help Irregular Heartbeat?

In conventional medicine, and indeed, in Western culture, the heart is seen as one of the most important, if not the most important, organ in the body. Not only does it supply the whole body with oxygenated blood, but it also is associated with our deepest emotions. TCM also views the heart as a central organ that governs the blood and vessels, and also the mind and spirit.
The traditional diagnostic methods employed by TCM practitioners can tell us a lot about the health of the heart. The feeling of the pulse gives us detailed information about the strength, quality, and speed of the heart rate. According to TCM theory, the heart “opens” out into the face, and so observing the pallor or color of the face, the brightness of the eyes, and the appearance, especially, of the tongue, also gives the acupuncturist vital information about the heart.
TCM providers classify different causes of irregular heartbeat by looking at the whole concert of presenting symptoms:
- Heart Qi deficiency or Blood deficiency: may happen after a long illness or loss of blood and be marked by heart palpitations, dizziness, memory problems, and/or insomnia. The pulse will be weak, and the tongue pale pink.
- Kidney yin deficiency with Heart Fire: chronic illness can deplete the kidneys so that they can no longer manage the balance of fluids and heat, so heat rises and disturbs the Heart. With this presentation, a person may be experiencing strong feelings of fear or anger, depression, ringing in the ears (tinnitus), and stomach problems.
Depending on the type of arrhythmia, the acupuncturist will choose acupuncture points and herbs to clear heat and dampness, nourish the blood, and calm and strengthen the heart. Specific herbal formulae work to activate and maintain blood flow, removing stasis, while also helping to protect the spleen and stomach.
A controlled study that compared patients with arrhythmias and tachycardias who were treated with medication (Lopressor) versus patients treated with both the medication and acupuncture and Chinese herbal formulations. The patients who received integrative care showed statistically very significant improvement over the patients using medication only.
A systematic review of randomized trials that compared acupuncture treatment versus typical medication treatment found that both types of treatment were equally effective for paroxysmal supraventricular tachycardia, that acupuncture in addition to medication was effective for ventricular premature beat, and that acupuncture was beneficial over no treatment at all for sinus tachycardia.
Acupuncture Near Me for Irregular Heartbeat
Unfortunately, cardiovascular disease is the leading cause of death among Americans. Over five million people in the U.S. experience atrial fibrillation, or heart flutter. The conventional methods of treating heart problems such as AFib and other types of arrhythmia can work, but they require people to become completely dependent upon medications or devices. These methods of treatment are also very expensive. Acupuncture and TCM offer an alternative or adjunct approach that can help improve heart function and restore a healthy heart rate without side effects.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.
How to Treat Lyme Disease With Acupuncture and TCM
By Xiaomei Cai, L.Ac., Ph.D. & Qineng Tan, L.Ac., Ph.D.

Red, circular rash that looks like a “bulls-eye?” Joint pain, muscle aches, and fatigue? These are signs that a person may have Lyme disease, an infectious disease that humans can contract when they are bitten by an infected tick. Lyme, a bacterial infection, can take a while to develop, and can cause chronic symptoms if it is not treated effectively. Acupuncture and TCM offer an alternative or adjunct way to help resolve the painful, debilitating symptoms of long-term Lyme disease.
Lyme disease is a type of bacterial infection transmitted by ticks. Ticks are parasitic arachnids, small spider-like creatures who bite other animals and feed on blood. If a tick is infected with a disease, it can infect the person or other animal it bites. Lyme disease, which is caused by the Borrelia burgdorferi bacterium, is just one of several infectious diseases that ticks can spread, including Rocky Mountain Spotted Fever (RMSF).
These critters are sometimes called “deer ticks” or “bear ticks” because they generally thrive in forest environments where they live symbiotically with these kinds of animals. But being bit by deer tick (tick on deer) doesn’t only happen in deeply wooded areas; anywhere that deer, squirrels, lizards, or birds may come into suburban areas, it is possible to be bitten by a tick. Actually, ticks, and therefore the infectious diseases they carry, are growing more prevalent because of humans encroaching into animals’ habitats. Tick bites most commonly occur in spring and summer.
Ticks do not fly; they can only get onto dogs or humans by crawling on them. This can happen quite easily if a tick is on a bush or other plant, and a person or dog brushes up against it. Ticks attach themselves to a host, and slowly suck their blood.
Lyme disease in dogs cannot be transmitted to humans, nor is lyme disease contagious, passing from human to human; you can only get Lyme disease by being bitten yourself. In order to pass Lyme disease to a person, a tick generally has to have been attached to that person’s skin for 36 hours or more. Ticks can be as small as the head of a pin, and they burrow in moist, hairy areas of their host’s body, so it is actually quite easy to have a tick on you without knowing it. After the tick drops off, a person may not feel anything at all, or only have a small, red bump that resembles a mild insect bite. In some cases, though, a person may feel right away that the area of the bite is hot, swollen, or causing a burning sensation.
If the tick was carrying Lyme disease, it can take several days to a few weeks for the more serious symptoms of Lyme to develop. Even then, the symptoms are not necessarily distinctive.
The early symptoms of Lyme disease can feel like a flu; fever, fatigue, aches and pains. Not everyone infected with Lyme will have the characteristic tick bullseye rash that develops around the site of the tick bite. When treated promptly with antibiotics, most cases of Lyme disease will resolve within a few weeks. However, many cases of Lyme disease are not diagnosed right away, and if it goes undetected, chronic problems can develop in the ensuing months. Once the bacteria has spread throughout the body, even a long course of antibiotics may not be able to get rid of it. Long-term Lyme symptoms may appear similar to other chronic inflammatory, autoimmune, or neurological conditions, such as fibromyalgia, Bell’s palsy, MS, chronic fatigue syndrome, or PTSD.
In extreme cases Lyme disease causes shoulder pain, hip pain, knee pain, fatigue, and other symptoms so severe that people can’t go about their regular daily routine. Sometimes diagnosis and treatment is further complicated by coinfections: concurrent other infections, that can also have been transmitted via the tick bite, or occur independently of it. Lyme and other tick-borne illnesses like RMSF can also trigger sepsis infections, which can be life-threatening, or lead to chronic pain, and/or PTSD (post-traumatic stress disorder). An MRSA skin infection (Methicillin-resistant Staphylococcus aureus), a type of staph infection that enters the skin through a wound, can develop around the infected tick bite; this staph skin infection is particularly resistant to antibiotics.
Unfortunately, symptoms of Lyme can become progressively worse over time, leading to disability and even death. Acupuncture and TCM offer an alternative for helping to heal Lyme disease, whether it is still in the early stages, or when it has become a chronic infectious disease.
Top 10 Symptoms of Lyme Disease

Signs of Lyme disease develop slowly, in stages, and can vary widely from person to person. Without the presence of the tell-tale bulls’ eye rash, both patients and doctors may have difficulty linking the spectrum of symptoms to a Lyme infection.
- Joint pain, swollen joins, arthritis
- Neuropathy, numbness or tingling, Bell’s palsy (face drooping)
- Fatigue
- Bulls-eye rash, also known as erythema migrans rash
- Headaches, migraines
- Sleep problems, sleep apnea, snoring
- Brain fog
- Trouble breathing
- Vertigo, dizziness
- Blurred vision
Other possible symptoms of Lyme include: ringing in the ears (tinnitus), heart palpitations, problems with memory and concentration, vision problems or inflammation around the eyes, and liver problems, like hepatitis. Symptoms of lyme disease in dogs are similar to those in humans, including stiff, swollen joints, tiredness, and loss of appetite.
Long-term effects of Lyme disease are sometimes referred to as “post-treatment Lyme disease syndrome.” Doctors are not sure why some people, even after being treated with antibiotics, seem to still be affected by long-term effects of Lyme disease.
Medical Diagnosis and Treatment of Lyme Disease
Getting a clear diagnosis of Lyme disease can be difficult. Currently, there is a two-step diagnostic process recommended to determine if a person has contracted Lyme disease. Two main kinds of tests can detect antibodies the body’s immune system creates to fight off the infection. However, it takes a while–at least several weeks, usually–for the body to build up enough of the antibodies that they become detectable. Often when people are aware early on that they may have been infected, and they get a test, it turns out to be negative. Usually, doctors try first one type of antibody test, and then the other to see if they get a positive result. Even then, medical science acknowledges that many (perhaps half of) Lyme disease cases are not detected this way.
A newer, still somewhat unproven form of testing involves taking a blood culture and trying to grow the bacteria that cause Lyme in a laboratory setting. This testing is more advanced and may be difficult for patients to access.
Once physicians have determined that Lyme infection is present, the usual treatment is a course of antibiotics that lasts a few to several weeks. In many cases, this seems to clear up the infection. In others, though, the antibiotics do not resolve the myriad symptoms patients are experiencing. Using antibiotics on a long-term basis is often not effective, and carries other risks to a person’s health.
Ongoing joint pain and inflammation is then usually treated with steroid medications or NSAIDS. Sleep problems and fatigue are often treated with antidepressants. These medications may help relieve symptoms temporarily, but they come with side effects, and do not address the root causes of the chronic symptoms of Lyme disease.
3 Stages of Lyme Disease
When early detection occurs, the Western medical approach of using antibiotics can often resolve Lyme disease within a few to several weeks. However, if the infectious disease is not found soon enough, Lyme disease will progress to more advanced stages. TCM methods can be helpful during all three stages of Lyme.
- First Stage Lyme disease – Within the first few weeks of the infection, and with early detection, antibiotics can be very helpful, working pretty well to stop the spread of the bacteria. However, because Lyme disease is often misdiagnosed, many people do not receive this treatment soon enough. During this phase, the symptoms are similar to those of the flu: chills, fatigue, heaviness in the limbs. As the infection moves in deeper, it can cause the skin rash, or hives. TCM treatment during the first stage will focus on clearing heat and detoxifying the body to rid it of infection.
- Second Stage Lyme disease – If the bacteria causing Lyme disease is not halted in its spread, it begins to affect the organs and the blood. The central nervous system and heart can become infected. These infections can last for months, and if not taken care of, can develop into the third phase. This is when a person may begin to feel joint aches, and arthritis-like symptoms. The body’s Qi and blood become deficient. Treatment with acupuncture and herbs at this point will work to help boost the Qi, clear heat and strengthen the whole immune system, and clear inflammation.
- Advanced stage Lyme disease – As the infection drags on, it can cause joint, skin, and nerve damage can take hold. Ongoing Qi and blood deficiency and stagnation cause fatigue, dizziness, insomnia, and memory loss.
A TCM provider will recognize what stage of Lyme disease a patient is in according to their symptoms, and customize the acupuncture points and herbal formulae used depending on their needs.
Acupuncture for Infectious Diseases

For millennia, TCM has recognized a type of disease that is caused by infection and can affect all systems of the body. We call this type of illness Gu zheng, or “Gu syndrome.” This classification covers illnesses caused by “invisible” pathogens, like viruses, funguses, and parasites. Along with the toxins from the tick bite, we consider how pathogens like heat, wind, and dampness all play a role in the illness. According to TCM theory, extreme heat in the body is also considered “toxic.” This category of condition helps us understand a variety of different systemic inflammatory illnesses, and gives us a framework for addressing each individual’s presenting symptoms.
One of the key features of Gu syndrome illnesses is how terrible and hopeless they can make people feel. Not only do people suffering from chronic inflammatory or immune-related conditions feel constantly tired and ache-y, but some of the sensations seem to come and go and feel so mysterious that they can’t be explained satisfactorily. If this is then compounded with the fact that many doctors don’t understand or know how to deal with the illness, it can leave patients feeling very frustrated and helpless. After months or years of this, debilitating physical symptoms may be accompanied by feelings of depression and anxiety.
A Yale Medical University study of patients, all in their 40s, suffering from long-term Lyme complications found that they had to reduce their activities, or even give up working, and doubted that they would ever recover. In interviews, patients made it clear that working with doctors who were more holistic was far preferred, and thus many had turned to CAM (complementary and alternative medicine) providers for help with Lyme disease.
Making a full recovery from long-term Lyme disease is possible, but it can take a long time to get rid of a bacterial infection that has woven itself deeply into the body’s organ systems. The benefit of Chinese herbal medicine for Lyme is that the powerful substances in the herbs can penetrate deep into the body at a cellular level. Working with an experienced acupuncturist means that your Chinese herbs for Lyme disease can be regularly updated, according to your individual needs, as you progress. This, in combination with acupuncture treatment for Lyme disease, moxibustion, and nutrition guidelines for an anti-inflammatory diet can all help patients feel better faster and prevent any further damage to the organs and the nervous system. Our TCM detox program may also be helpful.
Top 5 Tips for Lyme Disease Self-Care

Sometimes re-prioritizing health over all else is necessary in order to heal from a serious infectious disease.
- Conserve energy. Rest as much as possible.
- Drink extra water.
- Eliminate coffee, alcohol, spicy foods, chips, roasted nuts, any food that adds heat and inflames further. Try to reduce heat.
- Eat more cooling foods. Mung bean tea is an ideal choice.
- In the later stages of the disease, we may need to add more strengthening foods, like chicken stock and soup, and will recommend different herbal formulae, as well.
Overall, reducing stress and finding a meditation practice is helpful. For more detailed instructions on how to eat right to reduce inflammation, see our article specifically addressing anti-inflammatory food and lifestyle choices.
Acupuncture Near Me for Lyme Disease
Dealing with a complicated illness like Lyme disease is challenging for people and doctors. A long process of discovery and commitment may be necessary. Working with an experienced TCM provider gives patients the benefits of a multi-pronged, holistic way of addressing multiple symptoms, both physical and emotional. Acupuncture for infectious diseases like Lyme takes into account each patient’s individual concerns, and addresses the complex symptoms of Lyme in concert.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.