-
 Art of Wellness Acupuncture & Traditional Chinese Medicine (TCM)11704 Wilshire Blvd, Suite 295, Los Angeles, CA, 90025
Art of Wellness Acupuncture & Traditional Chinese Medicine (TCM)11704 Wilshire Blvd, Suite 295, Los Angeles, CA, 90025
myartofwellness@gmail.com310-451-5522 Office Hours
MonClosedTue7:30 am --4 pmWed7:30 am --4 pmThu7:30 am -- 4 pmFri7:30 am -- 4 pmSat7:30 am -- 4 pmSunClosedOur office opens from Tuesdays to Saturdays 7:30 am to 4 pm, will be closed on Memorial day, Independent day, Labor day, Thanksgiving day, Christmas and New year.
-
Recent Posts
- How to Treat Dysautonomia With Acupuncture and TCM
- How to Treat Myofascial Pain Syndrome With Acupuncture and TCM
- How to Treat Costochondritis With Acupuncture and TCM
- How to Treat Ankylosing Spondylitis With Acupuncture and TCM
- How to Treat Gastroparesis With Acupuncture and TCM
- How To Treat Sleep Apnea With Acupuncture and TCM
- How To Treat Baker’s Cyst With Acupuncture and TCM
- How to Treat Sinusitis With Acupuncture and TCM
- How To Treat Sjogren’s Disease With Acupuncture and TCM
- How to Treat Raynaud’s Syndrome With Acupuncture and TCM
- How to Treat Autoimmune Disorders With Acupuncture and TCM
- Chinese New Year 2024 Year of the Dragon
- Sign up to receive news and updates and get my free report:“The Top 10 Reasons to Try Acupuncture”

Uncategorized
How to Treat Dysautonomia With Acupuncture and TCM
By Qineng Tan, L.Ac., Ph.D. and Xiaomei Cai, L.Ac., Ph.D.

Fast heart rate or irregular heartbeat? Feel faint or dizzy when standing up? Fatigue, brain fog? Chest pain? These can all be Dysautonomia symptoms, or autonomic dysfunction. Acupuncture and TCM offer treatment for dysautonomia and autonomic neuropathy.
“Dysautonomia” is a general term that refers to multiple conditions related to autonomic dysfunction. There are many different types of autonomic nervous system disorders that fall under the umbrella of dysautonomia.
The autonomic nervous system (ANS) controls body functions like:
- Blood pressure
- Heart rate
- Breathing
- Digestion
- Temperature regulation
- Urinary function
- Sexual function
- Sweating
Basically, the ANS is in charge of all of the things our bodies do automatically—sometimes called involuntary functions—without us having to think about them.
Dysautonomia symptoms are fairly common, especially later in life, but medical science still has limited options for diagnosing and helping relieve these conditions.
Dysautonomia can be a primary condition, caused by genetic or degenerative disorders, or by damage to nerves (autonomic neuropathy). Secondary dysautonomia can occur as a result of another condition, such as an autoimmune disease, neurological disease, or injury.
Recent studies are beginning to show that dysautonomia, especially POTS, can be linked to long Covid. Even if a person had a Covid infection that was not particularly severe, the long-term effects of the virus have been shown to linger in the body, in the brain and nervous system, causing autonomic dysfunction long after the acute phase of the virus has passed.
TCM offers a way to treat dysautonomia, as acupuncture has been shown to have a positive effect on nervous system function.
Dysautonomia Symptoms
Different types of autonomic dysfunction will cause various symptoms in individuals. The most common symptoms of ANS include:
- Dizziness when standing up or changing position, light-headedness
- Vertigo
- Fainting, passing out
- Arrhythmia, irregular heartbeat, heart palpitations
- Fatigue, feeling tired
- Chest pain
- Shortness of breath
- Trouble swallowing
- Excessive sweating, or lack of sweating, clammy feeling
- Thirst
- Headaches, migraines
- Dry eyes, or excessive tears
- Digestive issues: constipation, diarrhea, etc.
- Frequent urination, incontinence
- Erectile dysfunction (ED)
- Sensitivity to sounds
Top 10 Types of Autonomia

Dysautonomia symptoms can seem similar to those of other nervous system conditions. This is why it can be difficult to be correctly diagnosed. It is fairly common for a person presenting with symptoms of dysautonomia to be told that they are suffering from anxiety or panic disorder.
Secondary dysautonomia occurs when another condition is the cause of symptoms. For example, dysautonomia systems can be the result of having disorders, such as:
- Parkinson’s disease
- Ehlers-Danlos Syndrome
- Celiac disease
- Guillain-Barre syndrome
- Lupus
- Lyme disease
- Sjogren’s syndrome
- Ulcerative Colitis
- Multiple Sclerosis (MS)
- Rheumatoid arthritis
- Sarcoidosis
- Crohn’s Disease
- IBS
- Fibromyalgia
These conditions can all cause damage to parts of the autonomic nervous system and therefore lead to symptoms of Dysautonomia.
There are at least 15 different types of Primary Dysautonomia. POTS is probably the most common one.
POTS Postural Orthostatic Tachycardia Syndrome – POTS is a condition characterized by an excessive increase in heart rate when moving from lying down to standing up (orthostatic intolerance). Symptoms may include lightheadedness, palpitations, fatigue, and fainting. It often affects young adults, particularly women.
Hyperadrenergic POTS is a subtype of POTS characterized by excessive sympathetic nervous system activity, leading to symptoms such as palpitations, anxiety, tremors, and hypertension in addition to orthostatic intolerance.
Treatment for POTS often involves a combination of lifestyle modifications, medications, and physical therapy. Lifestyle changes may include increasing fluid and salt intake to expand blood volume, wearing compression stockings to prevent blood pooling in the legs, and gradually increasing physical activity to improve cardiovascular fitness. Medications such as beta-blockers, fludrocortisone, midodrine, and pyridostigmine may be prescribed to help regulate heart rate, blood pressure, and blood volume.
IST Inappropriate Sinus Tachycardia – Inappropriate Sinus Tachycardia (IST) is a condition characterized by a fast heart rate at rest that is not caused by exercise, fever, or stress. It is considered inappropriate because the heart rate is elevated without a physiological reason. People with IST typically experience heart rates exceeding 100 beats per minute while at rest, often accompanied by symptoms such as palpitations, chest discomfort, fatigue, and shortness of breath.
The exact cause of IST is not fully understood, but it is believed to involve dysfunction in the sinus node, the natural pacemaker of the heart, which regulates heart rate. In individuals with IST, the sinus node may become overly sensitive to normal stimuli, leading to excessive firing and a rapid heart rate.
Treatment for IST focuses on controlling symptoms and improving quality of life. Lifestyle modifications like stress reduction, regular exercise, and avoiding triggers such as caffeine and nicotine may be recommended. Medications such as beta-blockers, calcium channel blockers, or ivabradine may be prescribed to help slow the heart rate and alleviate symptoms. In severe cases that do not respond to medication, procedures such as catheter ablation may be considered to modify the electrical pathways in the heart and reduce symptoms.
NCS Neurocardiogenic Syncope or Vasovagal Syncope – NCS, also known as vasovagal syncope, is a form of dysautonomia characterized by a sudden drop in heart rate and blood pressure, leading to fainting. It can be triggered by various factors such as prolonged standing, emotional stress, or pain.
Management of NCS focuses on avoiding triggers like prolonged standing, dehydration, or emotional stress, which can lead to fainting episodes. Increasing fluid and salt intake may help prevent episodes by expanding blood volume. Medications such as beta-blockers or fludrocortisone may be prescribed to help stabilize heart rate and blood pressure. In severe cases, implantation of a pacemaker or other cardiac device may be considered to regulate heart rhythm.
AAG Autoimmune Autonomic Ganglionopathy – AAG is a rare autoimmune disorder characterized by the production of antibodies that target autonomic ganglia, leading to autonomic dysfunction. Symptoms may include orthostatic hypotension, gastrointestinal dysmotility, and urinary dysfunction.
MSA Multiple System Atrophy – Management of MSA is focused on addressing specific symptoms related to autonomic dysfunction, parkinsonism, and cerebellar ataxia. Medications such as levodopa-carbidopa may be prescribed to alleviate motor symptoms, while medications such as fludrocortisone or midodrine may be used to manage orthostatic hypotension. Physical therapy and speech therapy may also be beneficial for managing motor and speech difficulties associated with MSA.
Management of MSA is focused on addressing specific symptoms related to autonomic dysfunction, parkinsonism, and cerebellar ataxia. Medications such as levodopa-carbidopa may be prescribed to alleviate motor symptoms, while medications such as fludrocortisone or midodrine may be used to manage orthostatic hypotension. Physical therapy and speech therapy may also be beneficial for managing motor and speech difficulties associated with MSA.
PAF Pure Autonomic Failure – PAF is a rare condition characterized by dysfunction of the autonomic nervous system, leading to problems with blood pressure regulation, heart rate variability, and temperature control. Symptoms may include orthostatic hypotension, urinary retention, and gastrointestinal issues.
Treatment for PAF aims to manage symptoms related to autonomic dysfunction. Lifestyle modifications like elevating the head of the bed, wearing compression garments, and increasing fluid and salt intake may help alleviate symptoms of orthostatic hypotension. Medications such as midodrine, fludrocortisone, and droxidopa may be prescribed to raise blood pressure and improve symptoms.
FD Familial Dysautonomia – begins at birth as a result of a genetic mutation inherited from the parents. FD affects the central nervous system, breathing, digestion, ability to form tears, regulation of temperature, regulation of blood pressure, taste, and pain sensitivity. Usually diagnosed in infancy, as babies will have trouble with feeding, will not cry tears, and will show poor growth. As the disease progresses, there may be development of arrhythmia, GERD, dry eyes and vision problems, scoliosis and/or weak bones.

DBHD Dopamine-Beta Hydrolase Deficiency – a rare genetic disorder characterized by the body’s inability to produce the enzyme dopamine-beta hydroxylase (DBH). This enzyme is essential for converting dopamine to norepinephrine, a neurotransmitter involved in regulating blood pressure and other autonomic functions.
Treatment for DBH deficiency focuses on managing symptoms by increasing fluid and salt intake to help maintain blood pressure, wearing compression garments to reduce symptoms of orthostatic hypotension, and avoiding triggers such as hot environments and prolonged standing.
In some cases, medications that increase blood volume or constrict blood vessels may be prescribed to help alleviate symptoms. However, treatment options for DBH deficiency are limited, and management typically involves ongoing monitoring and adjustment of therapies to address specific symptoms and complications as they arise.
OI Orthostatic Intolerance – Orthostatic intolerance (OI) refers to a group of conditions characterized by symptoms such as lightheadedness, dizziness, fatigue, and fainting when a person moves from lying down into an upright position.
There are various types of orthostatic intolerance, including postural orthostatic tachycardia syndrome (POTS), neurally mediated hypotension (NMH), and vasovagal syncope. Each type presents with its own set of symptoms and underlying mechanisms.
Besides lifestyle modifications such as increasing fluid and salt intake, wearing compression garments, and engaging in regular exercise can help improve blood flow and cardiovascular function, medications such as beta-blockers, fludrocortisone, and midodrine may also be prescribed to help regulate heart rate and blood pressure.
BF Baroreflex Failure – Baroreflex failure is a condition characterized by the inability of the body to regulate blood pressure in response to changes in posture or stress. It can result in symptoms such as orthostatic hypotension, hypertension, and fluctuations in heart rate.
Can Acupuncture Help Dysautonomia?

From the perspective of conventional medicine, dysautonomia is still considered a mysterious, confusing problem to solve. But TCM philosophy has recognized this type of disorder for many centuries. Acupuncture has been used since ancient times to help regulate the autonomic nervous system, although we have not always used that terminology for it.
A Chinese medical text that dates back to the first century B.C.E. describes “Ying-Wei Disharmony,” the symptoms of which include: breathing dysfunction, palpitations, irregular heartbeat, anxiety, digestive problems, nausea, dizziness, chronic pain, pressure headaches, tingling and numbness (neuropathy), and insomnia.
For a long time, medical science has looked for the mechanisms that make acupuncture work.
Recent studies have begun to show more clearly that the stimulation of acupoints affects the neural pathways, including the autonomic nervous system.
Acupuncture has been shown to help regulate ANS functions such as temperature regulation, blood pressure, heart rate, and muscle sympathetic nerve activities.
Acupuncture helps modulate transmitters in the brain, restoring balance when these activities have become dysregulated. More specifically, electro-acupuncture has been shown to work upon the hypothalamus, the medulla oblongata, the dorsomedial prefrontal cortex, and other regions of the brain that contribute to ANS function.
One study involving 30 female patients with dysautonomia symptoms showed that acupuncture treatment helped relieve heart palpitations, abdominal issues, and helped patients sleep better.
In addition to helping to regulate the autonomic nervous system, an acupuncturist will look for signs that other organ systems are out of balance and contributing to symptoms. For example, some patients with dysautonomia may need acupuncture and herbs to help balance the spleen and kidneys, which will in turn help improve adrenal function.
Stagnation of blood or phlegm can sometimes be causing blockages that contribute to nervous system dysfunction.
Acupuncture Near Me for Dysautonomia in Los Angeles Area
Dysautonomia is a complex condition to treat. A multi-faceted approach, combining conventional medical approaches with medications with acupuncture and herbal remedies can be helpful for managing the variety of symptoms a person may be experiencing. TCM is an excellent modality for working with this type of condition. If you or someone you know is struggling to get help for POTS or other autonomic disorders, call us at Art of Wellness in West L.A..
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.
How to Treat Myofascial Pain Syndrome With Acupuncture and TCM
By Xiaomei Cai, L.Ac., Ph.D. and Qineng Tan, L.Ac., Ph.D.

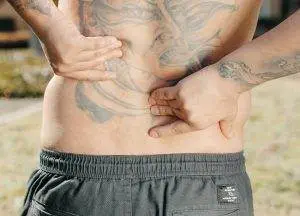
Muscle aches and pains? Knotted muscles? Pain in trigger points? These could be signs of myofascial pain syndrome. Acupuncture and TCM can provide myofascial release and help relieve chronic myofascial pain (MPS pain).
Myofascial pain disorder is a common, yet often overlooked chronic pain condition that affects the muscles and fascia. Fascia is the thin connective tissue that is found all over the body, holding muscles, organs, and blood vessels together. Fascia is also filled with nerves, which makes it highly sensitive.
Healthy fascia is thin, stretchy and pliable. Stress, injuries, weakness and other issues can cause fascia to tighten up, become sticky, dry, or thicker. This can cause painful knots to develop in your muscles.
These areas are sometimes called fascial adhesions, or myofascial trigger points, and they can be very tender to the touch and cause muscle soreness, aches and pains.
Chronic myofascial pain can seem very similar to fibromyalgia, or symptoms of ME/CFS, and is sometimes misdiagnosed as such. However, these conditions are distinct from one another.
Fibromyalgia causes widespread, diffuse pain and tenderness all over the body, while myofascial pain is centered around specific trigger point sites. Fibro, as it is sometimes called, is believed to be caused by a disorder within the central nervous system. Fibromyalgia is usually triggered by stress, trauma, hormonal changes, lack of sleep, or sensitivities to weather changes.
It has been suggested that long-term myofascial pain syndrome may ultimately lead to a person developing fibromyalgia, as the brain and nervous system become so used to experiencing pain that they begin to produce disordered pain signaling.
Acupuncture treatment, cupping, and therapeutic Chinese massage can provide trigger point therapy that is effective for relieving tight muscles and soreness.
Myofascial Pain Syndrome Symptoms

People experience myofascial pain differently from one another; each case is unique. For some people, the pain can come and go suddenly; for others, it’s a constant, dull pain.
Myofascial pain syndrome can feel like:
- Tight muscles, stiffness
- Throbbing pain
- Dull, aching pain
- Sore muscles, tender areas
- Knotted muscles, nodules or bumps in specific areas that are sore
- Muscle weakness
- Limited range of motion
- Trouble sleeping
- Headaches
- Fatigue
Myofascial pain can be localized in one area, or referred pain, which spreads to other nearby areas. Myofascial referred pain patterns can look like pain that originates in the rotator cuff which then spreads to the deltoid, and even down the arm to the hand.
What Causes Myofascial Pain?
Medical science is not entirely clear on the causes of myofascial pain syndrome, but it seems to occur more often in people who have experienced things like:
- Periods of inactivity, such as having one of your limbs in a cast
- Repetitive movements in your work
- Pinched nerves
- Injury to a muscle or muscle group
- Having to work outdoors in the cold
- Diabetic neuropathy
- Thyroid disorders, hypothyroidism
- Deficiencies in Vitamin D or folate, or iron deficiency
- Stress, chronic tension that leads to clenched muscles
- Structural conditions like scoliosis, spondylosis, or osteoarthritis
Estimates suggest that the majority of people who are treated for chronic musculoskeletal pain may have myofascial pain syndrome. Up to 85% of the general population may experience myofascial pain at some point in time.
Treatment for Myofascial Pain Syndrome
One of the primary approaches to managing myofascial pain syndrome is physical therapy. Physical therapists may use manual therapy, stretching exercises, and postural correction to address muscle imbalances, improve flexibility, and release tension in affected muscles. Trigger point therapy, which involves applying pressure to trigger points to release muscle knots and promote relaxation, is a common component of physical therapy for MPS.
Modalities such as heat therapy and cold therapy may also be used in conjunction with physical therapy to provide pain relief and enhance the effectiveness of treatment. Heat therapy helps to increase blood flow and promote muscle relaxation, while cold therapy can reduce inflammation and numb the affected area.
In addition to physical therapy and modalities, medications may be prescribed to manage pain and improve symptoms associated with myofascial pain syndrome. Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen may be recommended to reduce inflammation and alleviate pain. Muscle relaxants such as cyclobenzaprine or benzodiazepines may also be prescribed to help relax tense muscles and improve sleep quality. In some cases, tricyclic antidepressants or anticonvulsant medications may be used to modulate pain signals and improve overall pain management.
Trigger point injections are another treatment option for myofascial pain syndrome, particularly for individuals who experience severe or persistent symptoms that do not respond adequately to conservative measures. During a trigger point injection procedure, a local anesthetic or corticosteroid is injected directly into the trigger point to help alleviate pain and reduce muscle tension.
Acupuncture needling is also considered an effective and valuable treatment option for myofascial release and relief of musculoskeletal pain.
Can Acupuncture Help Myofascial Pain Syndrome?

Many studies conducted over the past two decades point to acupuncture as an effective mode of treatment for myofascial pain syndrome.
Acupuncture is effective for myofascial pain because it can positively affect the central nervous system, increase blood flow, increase endorphin production, improve fascial adhesions, and promote muscle relaxation. Acupoints used in TCM correspond closely with myofascial trigger points.
One study looked at patients who received two acupuncture treatments per week for four weeks on trigger points in the upper trapezius. Patients reported significant reduction in pain after just two weeks.
Another study followed two groups of patients with myofascial pain centered in the neck area. One group received acupuncture treatment. The other group had acupuncture and also engaged in regular aerobic exercise. Findings showed that both groups experienced significant improvement in pain symptoms.
A review of studies found that acupuncture was effective both for reducing myofascial pain and improving function and mobility.
Acupuncturists may also use electro-acupuncture, cupping, and massage techniques like gua sha and tui na to help move lymph and blood, release muscle trigger points, and improve muscular movement that has been limited by pain.
Acupuncture Near Me for Myofascial Pain Syndrome in Los Angeles
At Art of Wellness Acupuncture in West L.A., we have over 35 years of experience helping people find relief from musculoskeletal pain of all kinds. Dr. Tan and Dr. Cai are able to use electro-acupuncture, cupping, and massage techniques like Tuina for myofascial release. If you are suffering from muscle pain and tenderness, do not hesitate to make an appointment with us.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.
How to Treat Costochondritis With Acupuncture and TCM
By Qineng Tan, L.Ac. Ph.D. and Xiaomei Cai, L.Ac., Ph.D.

Chest pain? Rib pain, sternum pain? These can be costochondritis symptoms, caused by inflammation of the cartilage that connects the ribs to the sternum. Acupuncture and TCM can provide costochondritis treatment to relieve pain and inflammation.
Costochondritis is a pain condition caused by inflammation of cartilage in the rib cage. It can be scary, because the pain can feel like a heart attack or a symptom of heart disease.
It is quite common for people who are experiencing costochondritis pain to visit the emergency room complaining of chest pain. Almost 10% of ER visits are related to chest pain symptoms, and a significant number of those turn out to be related to something other than heart problems.
Sometimes called “chest wall pain syndrome,” or costosternal syndrome, costochondritis is considered a syndrome because it presents as a set of symptoms that often does not have a clear cause.
Possible causes of costochondritis include:
- Trauma or injury to the chest or ribs
- Persistent cough
- Repeated bouts of vomiting
- Chest or lung infection
- Allergies that affect the lungs
- Fibromyalgia
- Tietze syndrome
Suddenly doing some kind of heavy labor or intense workout that you’re not used to, that causes you to be winded, could cause inflammation of the chest. Playing contact sports in which you may be tackled or collide with another player or get hit hard with a ball in the chest could also cause costochondritis.
Tietze syndrome is a rare condition in which the cartilage connecting the ribs to the breastbone becomes inflamed and swollen. With Tietze syndrome, the pain and swelling in the chest is usually higher up, around the second and third ribs.
Costochondritis pain usually is felt more on the left side of the chest, radiating outward, and there isn’t any swelling involved.
Rib pain may be exacerbated when lying down, which can make it difficult to sleep comfortably.
Costochondritis is most commonly experienced by people in middle age (40-50s), but it can occur in children and adolescents, as well as adults.
In most cases, costochondritis is temporary. However, costochondritis pain can limit your activities and be debilitating for weeks, or even months. One study showed that up to a third of adults reported pain persisting beyond a year.
Acupuncture has been shown to help alleviate costochondritis pain, often in a matter of weeks.
Costochondritis Symptoms
Costochondritis pain can range anywhere from a slight tenderness to severe chest pain. In mild cases, the pain may go away in a matter of days, but in other cases, the pain can become serious.
Symptoms of costochondritis include:
- Sharp chest pain
- Chest pressure, chest ache, tenderness in breastbone
- Pain on the left side of chest, to the left of the breastbone
- Rib pain in more than one rib
- Pain radiating to shoulders and/or arms
- Chest pain when coughing, sneezing, or taking a deep breath
- Pain in chest when reaching up or twisting the torso
- Rib pain when lying down
- Pain when hugging someone
- Pain when putting on a seatbelt
Medical Diagnosis and Costochondritis Treatment

Other than the doctor palpating the area around your breastbone and ribs, there is no specific test to determine if you have costochondritis.
Chest pain can be an indicator of a variety of health conditions, including heart problems or lung problems, so it is always important to get it checked out with a healthcare professional. They will rule out other problems by ordering an EKG or chest X-ray in order to get to a diagnosis of costochondritis.
Treatment will consist of recommendations for ways to alleviate pain. Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (Advil, Motrin IB) or naproxen (Aleve) can help reduce inflammation and pain.
In cases of more severe or persistent pain, a doctor may prescribe stronger pain medications such as prescription-strength Motrin or muscle relaxers.
Applying heat or cold packs to the affected area can help reduce inflammation and alleviate pain. Some individuals find relief by alternating between heat and cold therapy.
In cases where pain is severe and not responding to other treatments, corticosteroid injections directly into the affected area may provide temporary relief by reducing inflammation.
Acupuncture treatment is a great way to relieve pain and reduce inflammation, without the side effects that can result from using pain medications or steroids for several weeks or months.
Can Acupuncture Help Costochondritis?

Acupuncture has been used for many centuries to treat pain and inflammation. Now, research is able to show how and why this modality is able to regulate inflammatory responses. Acupuncture affects the nerve signaling that produces hormones like dopamine and can reduce the production of cytokine storms. This is why acupuncture can help relieve inflammation and chest pain of costochondritis.
In TCM theory, pain and inflammation are usually considered to occur because of stagnation, or stasis, of blood and/or Qi (life force energy). The same symptoms can occur in different individuals because of different imbalances in the organs systems that are causing the blockages and different pathogenic factors, such as excess heat, dampness, etc.
Costochondritis inflammation can occur due to dampness and stagnation of Qi in the liver, spleen, and/or kidney systems. Depending on each patient’s specific situation, your acupuncturist will choose acupoints to open channels, clear dampness, heat, and phlegm. This allows for Qi and blood to flow smoothly again, cooling down the inflammation and relieving pain.
One case study of six women who were treated for costochondritis pain with acupuncture found that all patients reported improvement and were able to discontinue taking OTC pain medications.
One pediatric study looked at young students suffering from costochondritis; they were missing school, limiting their sports, dance, and work, and having trouble sleeping. After 4-6 weeks of acupuncture treatment, these patients reported a significant reduction in pain, and were able to resume their usual activities.
Not only is acupuncture treatment effective for relief of costochondritis pain; it can work quickly. In many cases, patients feel better after one or two treatments.
Acupuncture Near Me for Costochondritis in Los Angeles Area
Dr. Tan and Dr. Cai of Art of Wellness Acupuncture in West L.A. have been helping treat pain conditions for over 35 years. Our office is a home away from home where patients are able to relax and find relief from pain and inflammation. If you or someone you love is experiencing chest pain due to costochondritis, please do not hesitate to come in for a consultation.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.
How to Treat Ankylosing Spondylitis With Acupuncture and TCM
By Qineng Tan, L.Ac., Ph.D. and Xiaomei Cai, L.Ac., Ph.D.
Low back pain, morning stiffness, hip pain? Fatigue, losing weight, poor vision, skin rashes? These can all be signs of Ankylosing Spondylitis (AS). Ankylosing Spondylitis is a type of autoimmune arthritis. Acupuncture can help relieve Ankylosing Spondylitis symptoms like lower back pain.
Ankylosing spondylitis is a chronic inflammatory arthritis condition that most often affects the spine, usually the lower back and pelvis is an inflammatory disease; the primary symptom is inflammation in the sacroiliac joints, the joints where the base of the spine (the ilium) meets the pelvis (the sacrum).
Similar to rheumatoid arthritis (RA), ankylosing spondylitis is an arthritic condition triggered by a person’s immune system mistakenly attacking healthy tissues. Arthritis generally refers to pain and swelling in joint tissues.
Ankylosing spondylitis can also affect the hips, knees, shoulder joints, and/or the ribcage. When the body tries to heal affected bones, extra bone tissue begins to grow. This new bone growth is what causes joint stiffness and lack of flexibility. When the ribs are affected, it can restrict normal breathing.
Ankylosing spondylitis can, over time, weaken bones to the extent that they begin to collapse; these compression fractures can ultimately lead to curvature of the spine and a stooped posture. These fractures of the vertebrae can potentially affect the spinal cord and nerves.
“Ankylosis” is a term for the stiffening and fusion of bones. A “fused spine” can be the eventual outcome of Ankylosing spondylitis.
AS can also cause inflammation in the GI tract, causing gastrointestinal symptoms like diarrhea. In this sense, it is a type of inflammatory bowel disease (IBD).
In some cases, ankylosing spondylitis can cause eye inflammation, leading to vision problems like blurred vision, sensitivity to light, and painful eyes.
AS can also cause inflammation in the heart, which affects the function of the aortic valve and increases risk of heart disease.
As with other autoimmune disorders, modern medicine research has yet to discover what causes Ankylosing Spondylitis. Some gene mutations have been linked to ankylosing spondylitis, which is sometimes called axial spondyloarthritis.
Medical treatment for ankylosing spondylitis helps manage symptoms and slow the progression of the disease.
Acupuncture is widely recognized as an effective adjunct treatment for ankylosing spondylitis that can help reduce pain and improve mobility.
Top 10 Ankylosing Spondylitis Symptoms

The initial onset of symptoms of ankylosing spondylitis often includes episodes of lower back pain and stiffness or hip pain, which then may get more severe over time. But symptoms can vary widely from person to person, depending on which parts of the body are affected.
Symptoms of Ankylosing Spondylitis include:
- Persistent lower back pain and stiffness, typically worse in the morning and after periods of inactivity; back pain that improves with movement and exercise
- Pain and stiffness that radiate from the lower back to the buttocks, hips, and thighs, reduced flexibility and range of motion in the spine
- Hip pain, shoulder pain, chest pain, rib pain, knee pain, and/or ankle pain
- Difficulty taking deep breaths due to stiffness in the chest and ribcage
- Fatigue
- Bony fusion of vertebrae, leading to a stooped posture and loss of spinal mobility
- Eye inflammation (uveitis) causes eye pain, sensitivity to light, and blurred vision
- Loss of appetite, weight loss
- Psoriasis, skin rash
- Abdominal pain, diarrhea
There is usually a gradual progression of AS symptoms over time, potentially leading to severe spinal deformity and disability.
Conventional treatment, with acupuncture and TCM used as a complementary treatment, can be helpful for symptomatic relief.
Ankylosing Spondylitis Treatment
While there is no cure for AS, conventional medical treatments aim to manage symptoms, prevent complications, and improve quality of life for individuals with the condition.
NSAIDs such as ibuprofen, naproxen, and celecoxib are commonly used to reduce pain and inflammation associated with AS. They can help relieve symptoms and improve mobility, particularly during flare-ups.
Disease-Modifying Antirheumatic Drugs (DMARDs) like sulfasalazine and methotrexate may be prescribed to slow the progression of AS and reduce inflammation. These medications work by suppressing the immune system’s abnormal response, which contributes to inflammation, the formation of extra bone tissue, and damage to the joints.
Biologic drugs, such as tumor necrosis factor (TNF) inhibitors like adalimumab, etanercept, and infliximab, target specific components of the immune system involved in inflammation. They are often prescribed for individuals with moderate to severe AS who do not respond adequately to NSAIDs or DMARDs.
Physical therapy can play a crucial role in the management of AS by helping to improve flexibility, posture, and range of motion. Exercise programs tailored to the individual’s needs can help strengthen muscles, reduce pain, and maintain spinal mobility.
Orthopedic interventions, such as braces and orthotics, may be recommended to support proper posture and prevent spinal deformities caused by AS. In severe cases, surgical procedures like spinal fusion may be considered to stabilize the spine and alleviate pain.
Individuals with AS require regular monitoring by healthcare providers to assess disease activity, monitor medication effectiveness, and detect any complications early. Adjustments to treatment plans may be necessary based on disease progression and individual response to therapy.
Can Acupuncture Help Ankylosing Spondylitis?

Acupuncture and moxibustion have been used for centuries to help relieve joint pain and stiffness due to inflammation. In Chinese, conditions that might involve bone fusion are called “zhu jie yang,” which means “bamboo spine.”
According to TCM theory, the bones are nourished by the kidney system; we observe that the formation of AS symptoms occurs along the Kidney Meridian and the Governing Vessel meridian. Weakness in bones may be due to deficiency of kidney Qi and blockage of the Governing Vessel.
Painful areas arise when there are blockages in Qi. Blockages occur due to pathogenic forces of phlegm accumulation, cold, and dampness.
Acupuncture treatment, herbs, and moxibustion may be used to strengthen the kidneys, address kidney yang deficiency, and clear dampness and wind from the channels.
One study found that patients who were diagnosed with ankylosing spondylitis and kidney yang deficiency and were given acupuncture treatment and moxibustion focused on the Governing Vessel meridian experienced significant reduction of pain.
Moxibustion warms and invigorates yang energy and can help improve immune function. In the case of AS, this treatment protocol can help slow the progression of the disease, preventing inappropriate bone formation and reducing inflammatory responses.
A review of 26 studies that involved moxibustion treatment as an adjunct therapy for ankylosing spondylitis. The conclusion was that patients who had moxibustion in addition to conventional treatment fared better than those who did not receive moxibustion.
The British Acupuncture Council recommends TCM treatment for AS, as it has been shown to be effective at relieving back pain, without side effects.
One study of patients with ankylosing spondylitis who received acupuncture treatment and Chinese herb supplements, including herbal soak baths, found that people experienced pain relief and functional improvement.
A study that looked at 22 patients who received cupping therapy along with acupuncture and infrared heat lamps. The vast majority of the patients reported significant improvement in their pain symptoms.
Tuina therapeutic massage may also be helpful for helping to improve mobility and circulation.
A review of studies showed that acupuncture offers “unique advantages” in the treatment of ankylosing spondylitis, including localized pain relief, reduced inflammation, improvement of joint mobility, prevention of spinal deformity, and overall better quality of life.
Acupuncture Near Me for Ankylosing Spondylitis in West Los Angeles
Acupuncture can be an effective complementary treatment for many autoimmune disorders, including Sjogren’s disease, Lupus, as well as difficult-to-treat chronic pain conditions like fibromyalgia and complex regional pain syndrome (CRPS). Dr. Tan and Dr. Cai at Art of Wellness in West L.A. have over 35 years of experience helping patients find relief from all kinds of musculoskeletal pain.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.
How to Treat Gastroparesis With Acupuncture and TCM
By Qineng Tan, L.Ac., Ph.D. and Xiaomei Cai, L.Ac. Ph.D.

Bloated stomach, indigestion? Acid reflux, regurgitating food? Abdominal pain or nausea? These can be signs of gastroparesis, also known as stomach paralysis. Acupuncture and TCM can help relieve gastroparesis symptoms.
What is gastroparesis? Gastric paralysis is a functional problem that occurs when the stomach muscles and the nerves that are connected to them aren’t activating normally. Weak stomach contractions lead to delayed emptying of the stomach into the small intestine.
Gastroparesis impacts your digestion, triggering uncomfortable symptoms, and limiting your ability to get proper nutrition and keep your blood sugar levels steady.
There are different types of gastroparesis.
- Diabetes-related gastroparesis – a side effect of diabetes
- Post-surgical gastroparesis – occurs after surgery, such as gallbladder or pancreas surgery, gastric bypass surgery, stomach surgery for ulcer, or hysterectomy
- Idiopathic gastroparesis – occurs without a clear explanation
Most people experience idiopathic gastroparesis, which means that doctors cannot necessarily identify what causes gastroparesis in many cases.
Some medications can delay stomach emptying, including narcotic pain medications like codeine, morphine, or oxycodone. Medications that work on nerve signals, such as those used to treat overactive bladder, can delay gastric emptying.
Scleroderma, an autoimmune condition that affects collagen production and smooth muscle tissues, can lead to gastroparesis. Parkinson’s disease, which affects nerve signals, can lead to delayed emptying of the stomach. Hypothyroidism can also affect nutrition and digestion, as can eating disorders, metabolic disorders, and/or chronic fatigue.
Acupuncture is a good modality for helping to relieve gastroparesis symptoms, because it works on the nervous system, to help restore the proper signaling to muscles.
Rumination Syndrome
Gastroparesis is sometimes confused with “rumination syndrome.” Rumination syndrome refers to the regular regurgitation of undigested food. People with this syndrome often regurgitate undigested food back up shortly after a meal. This condition is usually related to the functioning of muscles of the diaphragm and unconscious behaviors around chewing and swallowing.
Gastroparesis Symptoms

The most common signs of gastroparesis are bloating, pain, nausea, and feeling full quickly when you eat.
Other symptoms of gastroparesis include:
- Feeling full quickly when eating
- Nausea, feeling nauseous after eating
- Vomiting, spitting up undigested food after eating
- Bloating, bloated stomach, abdominal bloating, abdominal cramping, stomach cramps
- Belching, burping
- Acid reflux, heartburn
- High blood sugar, low blood sugar
- Lack of appetite
- Weight loss
- Malnutrition
Gastroparesis needs to be addressed, as it can compromise your overall health by blocking you from getting proper nutrition from your food.
Gastroparesis Treatment
Medical treatment for gastroparesis will depend on which type a person seems to have. If a person has diabetes-related gastroparesis, for example, treatment will necessitate better management of blood sugar levels.
Initial diagnosis usually involves imaging tests to see what is happening with the stomach and if there may be a blockage. Gastric motility tests help doctors see how your stomach muscles are working.
People will often be advised to change their dietary habits: possibly following a liquid diet for a period of time, or eating smaller meals throughout the day. You may be told to avoid fats and fiber, as these macronutrients can contribute to delayed stomach emptying.
In some cases, intravenous feeding or tube feeding may be necessary, if a person is severely undernourished due to gastroparesis.
Antiemetic medications may be prescribed to help with nausea and vomiting. Proton pump inhibitors may be recommended to help with acid reflux symptoms.
There are some medications that can help promote better gastric emptying by stimulating more muscular contractions. Erythromycin and metoclopramide are two drugs used to treat gastroparesis. These medications can have side effects, like stomach cramps, nausea and constipation. They can also have negative interactions with other medications.
If these treatments are not helping, surgical options may be offered. A gastrostomy or may be inserted to help drain the stomach. A jejunostomy tube can be placed to bypass the stomach, so that nutrition gets into the intestines. A pyloroplasty is an operation in which the muscular valve of the stomach is widened.
Newer, experimental treatments involve placing electrodes on the stomach to help activate contractions. Botox injections have also been tried, as a way to calm spasms in the stomach.
Acupuncture treatment can help relieve gastroparesis symptoms without side effects or invasive procedures.
Can Acupuncture Help Gastroparesis?

According to TCM theory, gastroparesis can be caused by a deficiency of stomach and/or spleen Qi. Part of the TCM treatment protocol for gastroparesis might involve using herbs and certain foods to help warm and nourish the spleen. Acupuncture treatment can help improve muscular function, as well help to relieve stomach pain.
The motility of the gastrointestinal system is controlled by nerve and electric impulses. Acupuncture, and in particular, electro-acupuncture, can have a positive effect on stimulating electrical activity and restoring neural pathways within the body.
Acupuncture has been shown to be helpful for relieving many GI symptoms, like nausea and bloating. This makes it a good treatment for many types of gastric disorders and stomach problems.
In one study, three different groups of people were all given acupuncture treatment, with emphasis on different acupoints used for each group. All three groups of patients had significant improvement in their gastroparesis symptoms.
Specifically, testing with barium meal showed that acupuncture helped improve the speed of stomach emptying. Patients also reported positive changes in their feeling of fullness after a meal and experienced less bloating.
One case study of a woman in her 60s who had been suffering for two years with gastroparesis symptoms showed significant improvement of nausea, timely stomach emptying, and energy levels after just four acupuncture treatments.
Another case study of a man in his 60s who presented with symptoms of fullness, stomach pain and distension, with delayed stomach emptying, ended with complete resolution of his symptoms after eleven acupuncture treatment sessions.
Acupuncture Near Me for Gastroparesis in Los Angeles
At Art of Wellness in West Los Angeles, Doctors Tan and Cai have over 35 years of experience helping people find relief from all kinds of gastrointestinal symptoms and stomach problems, including: IBS, stomach ulcer, colitis, Crohn’s disease, diverticulitis, nausea, diarrhea, and constipation. It’s worth trying acupuncture to see if it can help relieve gastroparesis symptoms for you.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.