-
 Art of Wellness Acupuncture & Traditional Chinese Medicine (TCM)11704 Wilshire Blvd, Suite 295, Los Angeles, CA, 90025
Art of Wellness Acupuncture & Traditional Chinese Medicine (TCM)11704 Wilshire Blvd, Suite 295, Los Angeles, CA, 90025
myartofwellness@gmail.com310-451-5522 Office Hours
MonClosedTue7:30 am --4 pmWed7:30 am --4 pmThu7:30 am -- 4 pmFri7:30 am -- 4 pmSat7:30 am -- 4 pmSunClosedOur office opens from Tuesdays to Saturdays 7:30 am to 4 pm, will be closed on Memorial day, Independent day, Labor day, Thanksgiving day, Christmas and New year.
-
Recent Posts
- Chinese New Year 2026: Year of the Horse
- Acupuncture and TCM Treatment for Perimenopause Symptoms
- How to Treat Insulin Resistance With Acupuncture and TCM
- How to Treat Metabolic Syndrome With Acupuncture and TCM
- How to Treat Syncope With Acupuncture and TCM
- How to Treat Thoracic Outlet Syndrome With Acupuncture and TCM
- How to Treat Dupuytren’s Contracture With Acupuncture and TCM
- How to Treat Nutcracker Syndrome With Acupuncture and TCM
- How to Treat Rosacea With Acupuncture and TCM
- How to Treat Perioral Dermatitis With Acupuncture and TCM
- Lymphatic Drainage With Acupuncture and TCM
- How to Treat Turf Toe With Acupuncture
- How to Treat Nerve Pain With Acupuncture and TCM
- How to Treat Watery Eyes With Acupuncture and TCM
- How to Treat Ovarian Cysts With Acupuncture and TCM
- How to Treat Dystonia With Acupuncture and TCM
- Sign up to receive news and updates and get my free report:“The Top 10 Reasons to Try Acupuncture”

November 2025 M T W T F S S 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30
Traditional Chinese Medicine
How to Treat ADHD With Acupuncture and TCM
By Xiaomei Cai, L.Ac., Ph.D. & Qineng Tan, L.Ac., Ph.D.

Does my child have ADHD? Do I have ADHD? ADD/ADHD is a mental health disorder that causes children and adults to have problems with concentration, hyperactivity, or both. Trouble in school, problems at work, physical restlessness, mood swings, and frequent feelings of frustration can all be signs of ADHD in children and adult ADHD. Acupuncture and TCM offer a way to help symptoms of ADHD holistically, without the side effects caused by ADHD medications.
ADD stands for Attention-Deficit Disorder, referring to the poor concentration and problems staying on task that are often experienced by people with this neurodevelopmental disorder. Children and adults with ADD are easily distracted; they may appear to be “daydreaming” a lot of the time. ADHD stands for Attention-Deficit Hyperactivity Disorder, in reference to cases in which a person also exhibits impulsiveness, or difficulty sitting still. ADHD usually starts in childhood; often, ADHD symptoms carry over into adulthood and continue to cause problems if not addressed.
While ADHD in adolescents and children has been studied widely in recent years, the causes are still unknown. It is generally believed to be due to disordered biological processes occurring in the brain, and considered to be possibly genetic in origin. ADHD may be related to atypically low levels of chemical neurotransmitters like dopamine. Metabolism in the part of the brain that controls attention, movement, and social interaction appears to be different in brain imaging tests of children with ADHD.

For children with ADHD, this may lead to problems in school, even learning disabilities. Interrupting, not being able to wait their turn, fidgeting, and being forgetful or seeming “careless” are the obvious outward signs of ADHD that can make school challenging for children, and cause them to be considered disruptive in the classroom.
Adult attention disorder may show up as reckless behavior (traffic tickets, accidents, etc.), problems in relationships, trouble organizing things like paying bills or missing appointments, losing belongings, not being a “good listener,” or anger management issues.
According to current conventional medical thought, ADHD is considered a psychiatric condition: a product of chemical imbalance in the brain. ADHD in children is associated with behavioral problems that make it difficult to excel in school. Adults with ADD may have trouble finding success in their daily work and lives. For these reasons, people will consider getting medical treatment for ADHD. As with most psychiatric issues, treatment tends to focus on a combination of behavioral counseling and pharmacological intervention. Medications used to treat ADHD in both children and adults are stimulants that are thought to help boost attention span and a person’s ability to focus.
Acupuncture and TCM herbs can be used as an adjunct therapy or an alternative to medical treatment with drugs for ADHD in both children and adults.
Top 3 Types of ADHD:
ADD or ADHD symptoms manifest in a unique combination in each individual. Presentations of ADHD are divided into three categories:
- Inattentive/easily distracted type
- Hyperactive, impulsive behavior type
- Combined type, exhibits both inattention and hyperactivity
While boys are statistically more likely to be diagnosed with ADHD, this may have something to do with the fact that ADHD symptoms show up differently in girls than they do in boys. Parents and teachers may have a stronger tendency to explain girls’ behavior as being personality-based (“talkative” or “tomboy-ish”) rather than a serious problem worthy of attention. Girls may also be more likely to compensate for their ADHD, finding coping mechanisms that help them get along with teachers and appear to be OK, even if they are struggling with schoolwork or social problems.
ADHD and ASD (autism spectrum disorder) can often present in similar ways, and can coexist in some cases. Over half of people who have been diagnosed as autistic also show signs of ADHD, while about a quarter of people with ADHD are also considered to be on the autism spectrum. Some of the key differences between these two neurodevelopmental disorders are that children with ADHD are much more likely to show improvement in their behaviors as they grow up, and that people with ASD are more likely to exhibit “hyperfocus” rather than distraction.
When symptoms of ADHD are found in children, it is not unusual for parents to recognize that they, too, have faced similar struggles in their lives. Research suggests that about half of the time that a child is diagnosed with ADD or ADHD, at least one of their parents shows signs of the disorder, as well.
Top 10 Symptoms of Adult ADHD

Because ADD/ADHD is a mental health issue, it can be difficult to clearly identify. Many of the symptoms associated with ADHD are similar to those of anxiety. It is not uncommon for people with adult ADHD to also have anxiety or depression, so the conditions overlap.
- Trouble focusing on tasks or multitasking, poor concentration
- Impulsive behavior, recklessness
- Disorganization
- Poor time management skills, difficulty prioritizing or staying on topic
- Restlessness, sleep problems
- Easily frustrated
- Frequent mood swings
- Lose temper easily
- Difficulty articulating thoughts to others
- Difficulty coping with stress
Of course, everyone experiences some or all of these behaviors and emotions at some point in their lives. But if these problems began in childhood and continue to cause problems in daily life on an ongoing basis, then it may be due to adult ADHD.
Test for ADHD
Evaluation for ADHD is usually performed by a mental health professional, pediatrician, or family physician. There is no one specific test to determine if a child or adult has ADHD. Diagnosis is usually based on a comprehensive discussion with the patient and family members to determine whether a person displays 5-6 or more commonly recognized symptoms of ADD or ADHD, according to guidelines set by the American Psychiatric Association.
Brain imaging methods such as MRIs are used to conduct research about ADHD, but they are not part of a typical diagnostic process for the average person.
Medications for ADHD
Doctors commonly treat ADD or ADHD with stimulant medications that increase levels of dopamine and norepinephrine and are meant to help them focus better. These medications are based in amphetamine (Adderall, Dexedrine, etc.) or methylphenidate (Ritalin, etc.). Some are short-acting and need to be taken in 4-hour intervals; others are longer-acting, or designed to last all day.
While these medications are considered safe for children, they do not work in every case, and they carry a variety of side effects, including: changes in appetite, stomach problems, and sleep problems. These types of drugs constrict the blood vessels and can cause heart problems like arrhythmia, high blood pressure, and even heart attacks in some patients. They can also have a negative impact on mood and mental health, causing a child or adult to become even more irritable and/or anxious. In some cases, stimulant medications have been linked to suicidal ideation and aggressive behavior in children and adolescents.
Acupuncture for ADHD

TCM philosophy acknowledges the interconnectedness of the mind, spirit, and body. In the TCM view, problems like ADHD are concerned with imbalances of the Heart, the Mind, and the Shen (spirit or emotions). Pathogens like fire, wind, and dampness can invade the head, affecting the mind as well as the physical organs of the body.
Problems with concentration and restlessness stem from wind and excess heat in the head. Feelings of anger and frustration are often rooted in Liver Qi stagnation. Troubles with the appetite and digestion are often connected to deficiency in the Kidneys and Spleen. Thus, acupuncture treatment and herbal preparations will be designed to clear heat, get Liver Qi moving freely, and strengthen the Spleen and Kidneys.
The medications often prescribed to treat ADHD can actually have further negative effects on the heart and kidneys, causing deficiencies of Liver Qi and Kidney Qi.
A research study conducted with almost 600 children showed that acupuncture had an 84% efficacy rate. A study to test the effectiveness of electro-acupuncture on preschoolers with ADHD found not only that the majority of children showed improvement of symptoms, but that the improvement was still evident at a six-month follow-up.
Auricular acupuncture, in which points on the outer ear are stimulated with very tiny, thin needles or seeds that can be stuck to the ear and gently massaged daily, can be particularly effective for children, as it is very minimally invasive.
Certain herbs used in formulations to address attention deficits have been shown to help improve learning and memory.
Acupuncture Near Me for ADHD
If you or your child is struggling with attention deficits or impulsiveness, it can be stressful and scary to decide what to do about it. Poor concentration and hyperactivity can get in the way of doing well in school or work, and make it difficult to have positive social interactions and form relationships. It is certainly important to address these issues rather than ignoring them and hoping they’ll go away. However, many people are concerned that medications may have negative side effects, or be habit-forming. You may want to consider acupuncture as a natural way to address ADHD.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.
How to Treat TMJ With Acupuncture and TCM
By Qineng Tan, L.Ac., Ph.D. & Xiaomei Cai, L.Ac., Ph.D.
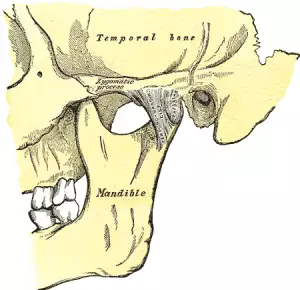
What is TMJ? “TMJ” is an acronym for “temporomandibular joint,” which is the double joint structure that attaches the lower jaw to the skull. “TMJ” is also used as a general term to refer to disorders of the jaw joint. Popping or clicking of the jaw joints, tension or pain in the jaw, grinding teeth, headaches, neck pain, and shoulder pain can all be signs of a TMJ disorder, or TMD. Acupuncture and TCM offer relief from TMJ jaw pain and inflammation.
The jaw joint is totally unique among joints in the human body in a few ways. It is really two joints that must always work together; you cannot choose to just move one side of your jaw. Also, the temporomandibular joint has two ways in which it moves; it “hinges,” and then, it “slides.”
Hinge joints, like the knees and elbows, allow flexion and extension on one plane, while remaining stabilized by a complex group of muscles, ligaments, and other connective tissues. Most of these joints are made of bones that are “molded” to fit and move together. Gliding joints, also called plane joints, like those in the ankles, wrists, and vertebrae, have flat sides that slide alongside each other when they move. The jaw joint combines both of these actions. Essentially the movement of the jaw is a kind of dislocation by design. Small discs of cartilage help to cushion the areas where the jawbone interacts with the sides of the skull in front of the ears.
It can be difficult to determine the exact causes of “TMD,” or temporomandibular disorders that cause pain and dysfunction. Injury to the jaw, dislocation of the jaw, inflammation of tissues, arthritis, and bruxism (clenching or grinding the teeth and jaw) can all potentially lead to jaw pain or clicking in the jaw. Erosion or damage to the cartilage sometimes causes TMD, impacting the usually smooth motion of the opening and closing of the jaw. Structural issues like missing teeth or an uneven bite can cause jaw problems. Dental and orthodontic work that requires the patient to hold the mouth open for long periods of time can sometimes lead to TMJ pain. Habitual movements like teeth grinding, biting on things like pencils, nail biting, or leaning your chin on your hand can also contribute to TMJ pain. Chronic pain syndromes like fibromyalgia can also cause jaw pain.
Most cases of TMJ disorders resolve themselves over time, usually within a few to several months. Resting the jaw and eating soft foods is usually recommended. Medical treatment usually involves medications to reduce inflammation and relieve pain while waiting for the jaw joint to gradually regain its normal function. Only in rare cases is surgery necessary to get rid of jaw pain.
TMJ, or myofascial pain in the muscles around the jaws, is experienced by a third or more of all adults at some point in their lives. TCM modalities like acupuncture can help alleviate the pain and impeded mobility of the jaw joint caused by TMJ disorders.
Top 10 Symptoms of TMJ

Pain around the jaw joints that comes and goes is the most common complaint of people with TMJ disorders. However, problems with the jaw can contribute to pain and tension in other parts of the head and shoulders, too. The most common signs of TMJ include:
- Pain in cheeks, tension in the jaw
- Jaw clicking, popping of jaw bones
- Limited movement of jaw, can’t open jaw normally
- Clenching of jaw, grinding teeth at night
- Tooth pain, pain in the back teeth
- Ear pain, ringing in the ears, tinnitus
- Headaches, migraines, pain behind eye, sensitive to light
- Stiffness in shoulders or neck, pain in neck, shoulder pain
- Numbness or tingling in arms, hands, or fingers
- Dizziness, vertigo
The combination of hard bony structures, muscles, and cartilage that are all involved in TMD causes TMJ pain that is hard to pinpoint because it may move around, and come and go. Most people describe the sensation as a dull ache. Some people don’t experience pain, but still have trouble with jaw clicking or opening and closing the jaw.
What Is the Treatment for TMJ?

A doctor or dentist may check for signs of TMJ by observing and manually examining the movement of the jaw joint. Dental X-rays may be used to help determine the cause of jaw pain. CT scan or MRI may be recommended to get a more detailed look at the bones and cartilage.
The primary recommendations for jaw pain and clicking is to rest the jaw as much as possible and eat only soft foods. Physical therapy (PT) can help strengthen the muscles of the face and encourage people to change habitual behaviors that might be contributing to TMJ. Wearing a splint or bite plate keeps the mouth and jaw in place and prevents grinding teeth in the night. This combination of PT and splinting is called stomatognathic treatment. If pain is serious enough to require further medical treatment, doctors will usually prescribe either pain relievers, anti-inflammatories, muscle relaxants, or some combination of these. Surgery is only used in rare cases when the jaw has become “locked,” or TMJ inflammation and pain has become chronic.
Acupuncture and TCM treatment offer a way to reduce inflammation and pain related to TMJ disorders without risky surgical procedures or the adverse side effects sometimes caused by corticosteroids and other medications.
Acupuncture Treatment for TMJ
Acupuncture can work to reduce inflammation and pain from many different conditions, including musculoskeletal disorders like TMD. Acupuncture is effective at reducing sensations of pain, both by reducing inflammation in areas from which the pain is originating and by stimulating the release of endorphins and other neurotransmitters that help boost feelings of well-being. Acupuncture treatment can also help the muscles involved with jaw function to relax, alleviating the “clicking” or “popping” associated with TMJ disorders.
In TCM theory, TMJ is often related to what we call different types of “obstruction” syndrome. Stress and trauma, both physical and emotional, can cause Qi stagnation and/or blood stagnation. Pathogenic forces like cold, heat, wind, and damp can cause painful obstruction, or blockages of energy and blood in certain areas of the body. People suffering from TMJ do not necessarily only have dental pain or myofascial pain, a clicking jaw, or limited movement. They may also be experiencing a variety of other symptoms that are actually related. A TCM practitioner will look at the whole picture of what each patient is feeling, and treat accordingly.

For example, a person with Liver Qi stagnation may have:
- tension in the facial muscles
- neck pain
- feelings of anger or anxiety,
- ringing in the ear, tinnitus
- headaches
A person with a Wind/Cold Bi Syndrome presentation might feel:
- acute onset of pain
- pain moves around from one area to another
- aversion to wind and cold
- fever, chills
- ear ache, ringing in the ears
As a holistic form of medicine, TCM works not only to relieve jaw pain and swelling, but to get to the root of the problem.
A comparative study designed to evaluate TCM treatment for TMJ found that patients who received acupuncture treatment reported less pain and muscle tenderness than those that did not.
A clinical study that compared groups of patients who received acupuncture treatment for TMJ pain and limited motion to patients treated with decompression splints. Both groups experienced reduction in pain and increased mobility, and the researchers concluded that acupuncture can be considered beneficial as either an adjunct or alternative treatment.
In some cases, a stiff, painful jaw joint can be a secondary symptom of another, more systemic problem like rheumatoid arthritis or fibromyalgia. These conditions can also be addressed with acupuncture.
Acupuncture Near Me for TMJ Disorders
TMJ disorders interfere with a person’s most basic activity: eating. While most cases of TMD improve within a matter of months with the proper rest, they can cause a lot of pain and frustration while a person is waiting to heal. Acupuncture and TCM herbs can help relieve TMJ pain and restore normal jaw function, helping people get back to normal more quickly than rest alone. At Art of Wellness, we have over 30 years of experience helping patients with musculoskeletal disorders and pain of all kinds find relief and a return to their usual mobility.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.
How to Treat Lyme Disease With Acupuncture and TCM
By Xiaomei Cai, L.Ac., Ph.D. & Qineng Tan, L.Ac., Ph.D.

Red, circular rash that looks like a “bulls-eye?” Joint pain, muscle aches, and fatigue? These are signs that a person may have Lyme disease, an infectious disease that humans can contract when they are bitten by an infected tick. Lyme, a bacterial infection, can take a while to develop, and can cause chronic symptoms if it is not treated effectively. Acupuncture and TCM offer an alternative or adjunct way to help resolve the painful, debilitating symptoms of long-term Lyme disease.
Lyme disease is a type of bacterial infection transmitted by ticks. Ticks are parasitic arachnids, small spider-like creatures who bite other animals and feed on blood. If a tick is infected with a disease, it can infect the person or other animal it bites. Lyme disease, which is caused by the Borrelia burgdorferi bacterium, is just one of several infectious diseases that ticks can spread, including Rocky Mountain Spotted Fever (RMSF).
These critters are sometimes called “deer ticks” or “bear ticks” because they generally thrive in forest environments where they live symbiotically with these kinds of animals. But being bit by deer tick (tick on deer) doesn’t only happen in deeply wooded areas; anywhere that deer, squirrels, lizards, or birds may come into suburban areas, it is possible to be bitten by a tick. Actually, ticks, and therefore the infectious diseases they carry, are growing more prevalent because of humans encroaching into animals’ habitats. Tick bites most commonly occur in spring and summer.
Ticks do not fly; they can only get onto dogs or humans by crawling on them. This can happen quite easily if a tick is on a bush or other plant, and a person or dog brushes up against it. Ticks attach themselves to a host, and slowly suck their blood.
Lyme disease in dogs cannot be transmitted to humans, nor is lyme disease contagious, passing from human to human; you can only get Lyme disease by being bitten yourself. In order to pass Lyme disease to a person, a tick generally has to have been attached to that person’s skin for 36 hours or more. Ticks can be as small as the head of a pin, and they burrow in moist, hairy areas of their host’s body, so it is actually quite easy to have a tick on you without knowing it. After the tick drops off, a person may not feel anything at all, or only have a small, red bump that resembles a mild insect bite. In some cases, though, a person may feel right away that the area of the bite is hot, swollen, or causing a burning sensation.
If the tick was carrying Lyme disease, it can take several days to a few weeks for the more serious symptoms of Lyme to develop. Even then, the symptoms are not necessarily distinctive.
The early symptoms of Lyme disease can feel like a flu; fever, fatigue, aches and pains. Not everyone infected with Lyme will have the characteristic tick bullseye rash that develops around the site of the tick bite. When treated promptly with antibiotics, most cases of Lyme disease will resolve within a few weeks. However, many cases of Lyme disease are not diagnosed right away, and if it goes undetected, chronic problems can develop in the ensuing months. Once the bacteria has spread throughout the body, even a long course of antibiotics may not be able to get rid of it. Long-term Lyme symptoms may appear similar to other chronic inflammatory, autoimmune, or neurological conditions, such as fibromyalgia, Bell’s palsy, MS, chronic fatigue syndrome, or PTSD.
In extreme cases Lyme disease causes shoulder pain, hip pain, knee pain, fatigue, and other symptoms so severe that people can’t go about their regular daily routine. Sometimes diagnosis and treatment is further complicated by coinfections: concurrent other infections, that can also have been transmitted via the tick bite, or occur independently of it. Lyme and other tick-borne illnesses like RMSF can also trigger sepsis infections, which can be life-threatening, or lead to chronic pain, and/or PTSD (post-traumatic stress disorder). An MRSA skin infection (Methicillin-resistant Staphylococcus aureus), a type of staph infection that enters the skin through a wound, can develop around the infected tick bite; this staph skin infection is particularly resistant to antibiotics.
Unfortunately, symptoms of Lyme can become progressively worse over time, leading to disability and even death. Acupuncture and TCM offer an alternative for helping to heal Lyme disease, whether it is still in the early stages, or when it has become a chronic infectious disease.
Top 10 Symptoms of Lyme Disease

Signs of Lyme disease develop slowly, in stages, and can vary widely from person to person. Without the presence of the tell-tale bulls’ eye rash, both patients and doctors may have difficulty linking the spectrum of symptoms to a Lyme infection.
- Joint pain, swollen joins, arthritis
- Neuropathy, numbness or tingling, Bell’s palsy (face drooping)
- Fatigue
- Bulls-eye rash, also known as erythema migrans rash
- Headaches, migraines
- Sleep problems, sleep apnea, snoring
- Brain fog
- Trouble breathing
- Vertigo, dizziness
- Blurred vision
Other possible symptoms of Lyme include: ringing in the ears (tinnitus), heart palpitations, problems with memory and concentration, vision problems or inflammation around the eyes, and liver problems, like hepatitis. Symptoms of lyme disease in dogs are similar to those in humans, including stiff, swollen joints, tiredness, and loss of appetite.
Long-term effects of Lyme disease are sometimes referred to as “post-treatment Lyme disease syndrome.” Doctors are not sure why some people, even after being treated with antibiotics, seem to still be affected by long-term effects of Lyme disease.
Medical Diagnosis and Treatment of Lyme Disease
Getting a clear diagnosis of Lyme disease can be difficult. Currently, there is a two-step diagnostic process recommended to determine if a person has contracted Lyme disease. Two main kinds of tests can detect antibodies the body’s immune system creates to fight off the infection. However, it takes a while–at least several weeks, usually–for the body to build up enough of the antibodies that they become detectable. Often when people are aware early on that they may have been infected, and they get a test, it turns out to be negative. Usually, doctors try first one type of antibody test, and then the other to see if they get a positive result. Even then, medical science acknowledges that many (perhaps half of) Lyme disease cases are not detected this way.
A newer, still somewhat unproven form of testing involves taking a blood culture and trying to grow the bacteria that cause Lyme in a laboratory setting. This testing is more advanced and may be difficult for patients to access.
Once physicians have determined that Lyme infection is present, the usual treatment is a course of antibiotics that lasts a few to several weeks. In many cases, this seems to clear up the infection. In others, though, the antibiotics do not resolve the myriad symptoms patients are experiencing. Using antibiotics on a long-term basis is often not effective, and carries other risks to a person’s health.
Ongoing joint pain and inflammation is then usually treated with steroid medications or NSAIDS. Sleep problems and fatigue are often treated with antidepressants. These medications may help relieve symptoms temporarily, but they come with side effects, and do not address the root causes of the chronic symptoms of Lyme disease.
3 Stages of Lyme Disease
When early detection occurs, the Western medical approach of using antibiotics can often resolve Lyme disease within a few to several weeks. However, if the infectious disease is not found soon enough, Lyme disease will progress to more advanced stages. TCM methods can be helpful during all three stages of Lyme.
- First Stage Lyme disease – Within the first few weeks of the infection, and with early detection, antibiotics can be very helpful, working pretty well to stop the spread of the bacteria. However, because Lyme disease is often misdiagnosed, many people do not receive this treatment soon enough. During this phase, the symptoms are similar to those of the flu: chills, fatigue, heaviness in the limbs. As the infection moves in deeper, it can cause the skin rash, or hives. TCM treatment during the first stage will focus on clearing heat and detoxifying the body to rid it of infection.
- Second Stage Lyme disease – If the bacteria causing Lyme disease is not halted in its spread, it begins to affect the organs and the blood. The central nervous system and heart can become infected. These infections can last for months, and if not taken care of, can develop into the third phase. This is when a person may begin to feel joint aches, and arthritis-like symptoms. The body’s Qi and blood become deficient. Treatment with acupuncture and herbs at this point will work to help boost the Qi, clear heat and strengthen the whole immune system, and clear inflammation.
- Advanced stage Lyme disease – As the infection drags on, it can cause joint, skin, and nerve damage can take hold. Ongoing Qi and blood deficiency and stagnation cause fatigue, dizziness, insomnia, and memory loss.
A TCM provider will recognize what stage of Lyme disease a patient is in according to their symptoms, and customize the acupuncture points and herbal formulae used depending on their needs.
Acupuncture for Infectious Diseases

For millennia, TCM has recognized a type of disease that is caused by infection and can affect all systems of the body. We call this type of illness Gu zheng, or “Gu syndrome.” This classification covers illnesses caused by “invisible” pathogens, like viruses, funguses, and parasites. Along with the toxins from the tick bite, we consider how pathogens like heat, wind, and dampness all play a role in the illness. According to TCM theory, extreme heat in the body is also considered “toxic.” This category of condition helps us understand a variety of different systemic inflammatory illnesses, and gives us a framework for addressing each individual’s presenting symptoms.
One of the key features of Gu syndrome illnesses is how terrible and hopeless they can make people feel. Not only do people suffering from chronic inflammatory or immune-related conditions feel constantly tired and ache-y, but some of the sensations seem to come and go and feel so mysterious that they can’t be explained satisfactorily. If this is then compounded with the fact that many doctors don’t understand or know how to deal with the illness, it can leave patients feeling very frustrated and helpless. After months or years of this, debilitating physical symptoms may be accompanied by feelings of depression and anxiety.
A Yale Medical University study of patients, all in their 40s, suffering from long-term Lyme complications found that they had to reduce their activities, or even give up working, and doubted that they would ever recover. In interviews, patients made it clear that working with doctors who were more holistic was far preferred, and thus many had turned to CAM (complementary and alternative medicine) providers for help with Lyme disease.
Making a full recovery from long-term Lyme disease is possible, but it can take a long time to get rid of a bacterial infection that has woven itself deeply into the body’s organ systems. The benefit of Chinese herbal medicine for Lyme is that the powerful substances in the herbs can penetrate deep into the body at a cellular level. Working with an experienced acupuncturist means that your Chinese herbs for Lyme disease can be regularly updated, according to your individual needs, as you progress. This, in combination with acupuncture treatment for Lyme disease, moxibustion, and nutrition guidelines for an anti-inflammatory diet can all help patients feel better faster and prevent any further damage to the organs and the nervous system. Our TCM detox program may also be helpful.
Top 5 Tips for Lyme Disease Self-Care

Sometimes re-prioritizing health over all else is necessary in order to heal from a serious infectious disease.
- Conserve energy. Rest as much as possible.
- Drink extra water.
- Eliminate coffee, alcohol, spicy foods, chips, roasted nuts, any food that adds heat and inflames further. Try to reduce heat.
- Eat more cooling foods. Mung bean tea is an ideal choice.
- In the later stages of the disease, we may need to add more strengthening foods, like chicken stock and soup, and will recommend different herbal formulae, as well.
Overall, reducing stress and finding a meditation practice is helpful. For more detailed instructions on how to eat right to reduce inflammation, see our article specifically addressing anti-inflammatory food and lifestyle choices.
Acupuncture Near Me for Lyme Disease
Dealing with a complicated illness like Lyme disease is challenging for people and doctors. A long process of discovery and commitment may be necessary. Working with an experienced TCM provider gives patients the benefits of a multi-pronged, holistic way of addressing multiple symptoms, both physical and emotional. Acupuncture for infectious diseases like Lyme takes into account each patient’s individual concerns, and addresses the complex symptoms of Lyme in concert.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.
How To Treat Amnesia With Acupuncture and TCM
By Qineng Tan, L.Ac., Ph.D. & Xiaomei Cai, L.Ac., Ph.D.

Are you experiencing unusual forgetfulness? Amnesia due to an injury or a brain disease like Alzheimer’s can cause loss of memory. TCM and acupuncture offer an alternative treatment for problems with memory loss due to different types of amnesia or dementia related to brain diseases like Alzheimer’s or Parkinson’s.
Amnesia is often depicted in stories as the sudden loss of one’s memory, or even their whole identity, due to a traumatic accident of some sort. That kind of dramatic memory loss is rare in real life. Difficulty remembering events from one’s past is called retrograde amnesia. The most common type of amnesia, however, is anterograde amnesia, which causes short-term memory problems. People with anterograde amnesia may be able to remember facts they learned in school, and how to do things like play a sport or an instrument, but they have trouble remembering what they did earlier this morning, or what day of the week it is. Anterograde amnesia can have a serious impact on a person’s life, as it can make it difficult to retain new information, learn new skills, or form relationships with new people.
Conditions like Alzheimer’s and Parkinson’s can affect memory and cause other types of cognitive impairment. Memory problems can be a part of dementia; the term “dementia” encompasses other kinds of cognitive decline in addition to memory loss. Being more forgetful is considered a common aspect of mild cognitive impairment (MCI). MCI is the term for changes in thinking patterns that occur in older adults, sometimes as a precursor to more serious dementia. “Amnestic MCI” pertains to short-term memory problems like forgetting recent events, appointments, and facts or names one might have been able to call up easily in the past.
People suffering from depression and/or anxiety, and those with PTSD often experience short-term memory loss, forgetfulness, or a sense of confusion.
At this point, there is no real medical solution for amnesia or other kinds of memory loss. There are no treatments that cure or reverse dementia or Alzheimer’s. Medications like cholinesterase inhibitors and memantine may help to slow the breakdown of certain neurotransmitters–brain chemicals that relate to memory and learning capacity. Cognitive therapy can help people work on their memory skills and teach them coping mechanisms, like using various forms of reminders and creating stable routines that help them continue to perform their daily tasks.
Research has shown that TCM and acupuncture treatment have a positive impact on cognitive impairment, as measured both by memory assessments, as well as the impact on neurotransmitter activity in the brain.
Top 5 Types of Amnesia

Amnesia is classified into two main categories: neurological amnesia and functional amnesia. Neurological amnesia is caused by some type of physical problem with the brain, either due to an injury, a stroke, a tumor, or diseases like Alzheimer’s and Parkinson’s. Amnesia could also result from an infection that affects the brain, such as HIV, Lyme disease, or encephalitis. Functional amnesia is caused by some psychologically damaging event that causes a person to “block out” memories. This type of amnesia is considered a psychiatric disorder.
- Retrograde amnesia – this type of amnesia occurs after a traumatic event or injury to the brain. It affects memories that were stored before the inciting event, but not necessarily the entire history of memories. Usually the events leading up the trauma are the ones that are compromised.
- Anterograde amnesia – this type of amnesia causes short-term memory loss. While a person can still pay attention, they have trouble retaining new information or forming new memories related to current events.
- Transient global amnesia – this type of amnesia incorporates both retrograde and anterograde types of memory loss, but only for a short period of time (anywhere from a few to 24 hours). This temporary loss of memory usually occurs in older people, perhaps because of some loss of blood flow to the brain (ischemia) or loss of oxygen to the brain (hypoxia), or even because of a seizure.
- Dissociative amnesia – a mental health disorder in which a person blocks out memories or certain facts about their life after an emotionally traumatic event. This is sometimes known as “selective amnesia.”
- Infantile amnesia – (or childhood amnesia) this term refers to the fact that most people do not have memories from the early years of their life.
Other factors that can affect memory to the extent that they cause amnesia are severe alcoholism (when a person gets “blackout drunk” and cannot remember what has happened), severe nutritional deficiencies, thyroid issues, or exposure to radiation. Some drugs, like benzodiazepines, or anti-epileptic medications, can cause memory loss while the drug is in effect. Electroconvulsive Therapy (ECT) is sometimes used in psychiatric treatment to induce selective amnesia.
Sometimes amnesia is temporary, such as after an injury. Once the brain heals, memory will often be restored. Amnesia due to brain damage, such as after a stroke, may be permanent, while amnesia caused by a degenerative disease like Alzheimer’s, may be progressive in nature. Acupuncture treatment can be beneficial for people with various types of memory loss, both by helping people heal after brain trauma, and helping to protect the brain and other organs from degeneration due to aging or other kinds of disease.
Can Acupuncture Help Amnesia?

TCM theory takes a different view of the organ systems of the body than conventional modern medicine does. Whereas memory loss, cognitive impairment, amnesia, and dementia are seen as primarily having to do with the brain, in TCM we see problems with memory and cognition as also being related to the function of the kidneys, liver, spleen, and heart. The kidneys, in particular, are believed to support the brain, so if the kidneys are weak, or congested with phlegm, this can lead to amnesia. The buildup of phlegm in the body can block the smooth flow of qi and blood, leading to a lack of nourishment to the brain. It can also block the channels of communication between the heart and the brain. This concept of phlegm is roughly analogous to the conventional medical view of how heart disease arises from the buildup of cholesterol clogging the arteries. TCM treatment for amnesia and dementia will often focus, then, on the clearing of phlegm from the channels, and working to resolve other conditions, like high blood pressure or diabetes, that are contributing to the problems of memory loss and cognitive deficits.
Herbs have been used for many centuries in TCM to help improve memory function and stave off cognitive decline. In recent years, scientific research has begun to confirm that these herbs can work to reduce neurodegeneration. TCM herbal formulations have the benefit of being highly customizable, while being relatively free of potential negative side effects. Acupuncture has been demonstrated to help patients recover neurological function after traumatic brain injuries.
Top 5 Tips for Improving Your Memory With TCM
Stimulating more blood flow to the brain can help boost your memory. Try these simple home remedies to help promote better cognitive function.
- Acupressure Points for Memory – Find the tender spot right in the center of the top of the head. Stimulate this point, and the four points that can be found one inch away from the center in each direction: right, left, front, and back (see photo above). Apply gentle but deep, downward pressure with your finger to each of these five points 50-60 times each day.
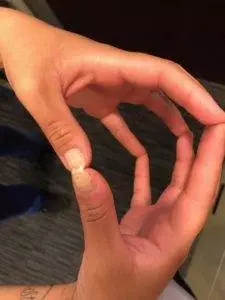
- Stimulate the Fingertips and Tips of the Toes – Hold the hands so that the tips of the fingers and thumbs touch. Gently press or stroke the corresponding fingers together, each stimulating the other, up to a hundred times. Practice daily. Similarly, gently press/stroke the tip of each toe, up to a hundred times per day.
- Keep the Neck Supported – when the neck is stiff or out of alignment, blood flow to the head and brain may be compromised. If you have neck pain or tightness, be sure to address it adequately with acupuncture, a supportive pillow and appropriate sleeping position, and gentle exercise.
- Dry Brush the Scalp – use a brush or comb to stimulate the whole scalp every day. This will help bring good blood flow to the head.
- Massage the Ears – gently knead the whole outer ear, especially the ear lobe, until it is warm and red. This will stimulate many beneficial acupressure points located on the ear.
Acupuncture Near Me for Memory Loss
Perhaps someone close to you has begun to show worrying signs of cognitive decline or loss of memory. People who are suffering from amnesia and dementia associated with degenerative brain diseases like Alzheimer’s can benefit from an integrative approach that includes acupuncture and herbs.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.
How to Treat Heel Pain With Acupuncture and TCM
By Qineng Tan, L.Ac., Ph.D. & Xiaomei Cai, L.Ac., Ph.D.
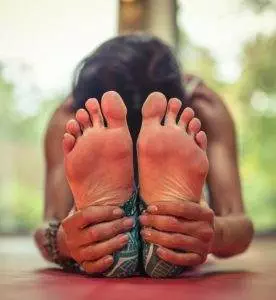
Chronic bottom of heel pain, especially when you first get up in the morning? Heel pain can be due to plantar fasciitis, an inflammatory condition of the large ligament that supports the arch of the foot. Bone spurs in the foot (heel spur), Achilles tendonitis, and bursitis can also cause pain in back of heel. Acupuncture and TCM treatment offer relief from chronic plantar fasciitis pain and achilles tendon pain.
Experiencing stiffness or pain in the heel when you first get up in the morning is a sign of plantar fasciitis. The sensation may improve as you warm up and move more throughout the day, or you may have severe, burning pain whenever you put your weight on the back part of your foot. The plantar fascia provides shock absorption and cushioning for the heel; when it is overused, small microtraumas and tears lead to inflammation. People with very flat feet, fallen arches, or very high arches are more prone to plantar fasciitis, as are older people.
Stiffness above the heel is an indication of Achilles tendinitis. When the tendon that connects the muscles of the calf to the heel bone is strained, it can cause an aching sensation or pain in the back of the heel. This usually happens because of sudden overuse, like when a person decides to go for a long run when they haven’t exercised in a while, or when their sneakers are worn out. Achilles tendinitis is more common in men, and in people with high blood pressure.
Stiffness in the ankle and side of foot pain can be due to posterior tibial tendonitis, which can develop when the heel bone shifts in such a way as to put extra stress on the outside of the ankle.
Heel spurs–extra bone tissue on the bottom or back of the heel–develop due to over-stress of the foot. In most cases, the bone spurs on the foot don’t cause pain in and of themselves, but they often coincide with either plantar fasciitis or Achilles tendonitis, and the conditions aggravate each other.
TCM modalities of acupuncture, electro-acupuncture, moxibustion, and herbal formulae have been shown to help relieve heel pain and inflammation due to all types of conditions, including plantar fasciitis and Achilles tendinopathy.
Top 5 Heel Pain Causes

Pain in the heel and other types of bottom of foot pain can be due to one of or a combination of several different types of conditions:
- Plantar fasciitis – about 2 million people are diagnosed in the U.S. each year with plantar fasciitis, which occurs when the connective tissues that support the bottom of the foot become inflamed, usually from repetitive use or being overloaded. Some athletes are prone to this type of inflammation due to constant stress on the foot. Health conditions like obesity and diabetes also make people more susceptible to plantar fasciitis heel pain. While this type of heel pain walking is generally attributed to inflammation, it is also due to the natural degeneration of collagen that occurs with age, making the connective tissues weaker and more brittle.
- Heel spur – (bone spurs foot) refers to the extra growth of bone tissue on the bottom of the calcaneus (bone spur heel). Heel spurs often grow as the body’s reaction to plantar fasciitis; the two conditions can exist together or separately. Sometimes people with heel spurs aren’t aware of them, but bone spurs foot can cause sharp bottom of foot pain. Heel spurs often develop because of the stress of running or jogging, or wearing improper footwear. Posterior calcaneal exostosis, colloquially known as “pump bump”, is when there is abnormal growth of bone tissue on the back of the heel, usually due to wearing a certain style of shoe (pumps or high heels).
- Bursitis – Bursa are small sacs of fluid that help to provide cushioning in various joints of the body. Calcaneal bursitis occurs when the bursae that sit between the Achilles tendon and the heel bone become inflamed. Heel bursitis is usually caused by too much impact on the ankle joint and heel while running or by wearing shoes that create a lot of pressure on the back of the heel.
- Achilles tendonitis – (also spelled achilles tendinitis) When the tendon that runs from the heel up the back of the lower leg becomes inflamed, often due to a lot of jumping movements, it can create pain and stiffness in the back of the heel. This overuse injury is very common in middle aged adults who engage in sports like tennis or basketball only sporadically, and may not warm up adequately before running and jumping.
- Gout – an arthritic condition in which a buildup of uric acid crystals causes swelling and pain in the joints of the foot.
Pain in the heel can also be caused by a pinched nerve, or compression of the plantar nerve, or by bruising on the heel. Peroneal tendonitis, when the tendon that runs along the side of the ankle and then under the foot becomes inflamed and swollen, can also cause pain in the back of the heel. Sciatic nerve pain can also cause radiating pain that shoots down the leg and causes pain in the foot.
What Is the Treatment for Plantar Fasciitis?
Conventional clinical medicine considers plantar fasciitis to be a self-limiting condition, which means that it will eventually improve on its own, with rest and modifications of movement. Doctors will usually recommend that people cease weight-bearing activities as much as possible. This can be extremely frustrating for patients, though, as it often means being advised to rest the foot for six to eighteen months. Physical therapy for plantar fasciitis that focuses on stretching and strengthening the plantar ligament may be recommended. Special orthotics, arch supports, or heel cups that provide cushioning can be helpful. Night splints are sometimes used to keep the foot and ankle in a position that keeps the ligament on the bottom of the foot stretched long, rather than shortened, while sleeping.
For heel pain relief, doctors may administer steroid injections and other anti-inflammatory medications. Steroid injections do carry some risks; about one out of ten patients treated this way for plantar fasciitis pain experience a rupture of the plantar tissues, which can lead to an even more severely chronic condition. Of course, the problem with taking NSAIDS on a regular basis is that they can cause problems with the stomach lining and gastro-intestinal bleeding. If rest and other methods do not improve the situation after many months, then surgical release of the plantar fascia may be considered.
Achilles tendonitis treatment is usually similarly conservative, involving rest and pain relievers. Unfortunately, recovery from the heel pain caused by plantar fasciitis or Achilles tendinitis is often a long, tedious process of abstaining from physical activity. For many people, whether they have jobs that require them to be on their feet or simply enjoy engaging in sports, it may feel impossible to stick to the standard treatment program. Acupuncture treatment offers a way to help relieve pain and inflammation and speed the healing of plantar fasciitis.
Acupuncture for Heel Pain

TCM takes a holistic view of pain conditions such as heel pain. While undoubtedly heel pain is caused largely by inflammation in the soft tissues of the foot and calf, there are often other underlying factors that cause these kinds of injuries to happen to people in middle age. In TCM philosophy the kidneys are believed to provide support and nourishment to the bones; this concept is called “kidney governing bone.” Heel pain and heel spurs occur due to deficiencies or excesses of the kidney Qi. Soft tissues such as the plantar ligament and the Achilles tendon are governed by the liver. Thus, acupuncture treatment for heel pain, heel spurs, plantar fasciitis, and Achilles tendinitis will often involve using acupoints to strengthen and tonify the Kidney Qi and Liver Qi.
Acupuncture is known to be effective for helping to relieve pain due to inflammatory conditions of all kinds, and also for helping to increase the production of collagen, which helps to keep the connective tissues of the foot and calf strong and supple. Acupuncture helps the healing of ligaments and tendons by improving reducing inflammation, improving blood flow and cell repair. The ancient textbook of Chinese medicine, The Yellow Emperor’s Classic of Internal Medicine, even describes a specific acupuncture technique used to promote healing in the Achilles tendon.
Herbs can be used both internally and externally to help heel pain. An herbal formula that is steeped in warm water and used as a daily foot soak can be especially helpful for relieving swelling in the heel and pain in the bottom of the foot.
One research study compared patients treated with corticosteroid injections for plantar fasciitis versus patients treated with acupuncture. Six months later, the patients who had steroid shots reported a 76% effective rate, while the patients who’d had acupuncture reported a 97% effective rate.
A hospital study compared two groups of patients – some treated with integrated protocol of acupuncture and warm herbal foot baths, and the others treated with the herbal foot baths only. The effective rate for the foot-soaking only was 69%, and the effective rate jumped up another 22% for the patients who also had acupuncture.
A systematic review of four studies involving acupuncture for patients with plantar fasciitis heel pain showed a significant reduction in pain after 4-8 weeks of treatment.
Top 5 Tips for Heel Pain

Prevention of heel pain involves mindfulness around your preparations for physical activity. The right gear and the regular practice of plantar fasciitis exercises can help prevent injury to the tendons of the foot.
- Wear good-fitting, properly supportive shoes – whenever you walk, run, or work out. Replace them regularly, even if you haven’t worn them much, because cushioning materials can break down over time, even when the shoes are just sitting in your closet.
- Warm up – taking the extra time to warm up before and cool down after running and jumping is always important, for all of the muscles of the body, but especially for the feet and lower legs. Be sure to adequately warm up the calf muscles, and stretch them before and after your primary workout.
- Vary your workout – cross-training, which means alternating different types of activities, not only helps to improve your overall cardiovascular and muscular fitness, but it also prevents repetitive use injuries that can occur when you run every day. Focus on resting the feet some days, by riding your bike or swimming instead of running or doing high-intensity aerobics.
- Soak your feet – before bed, soak heels in warm water to help improve circulation.
- Manage your weight – Heel pain is usually related to how much pressure the foot has to withstand on a daily basis. Maintaining a lower body weight will help take the pressure off the heels. Losing weight while being asked to stay off your feet can be especially difficult, so talk with your TCM provider about a healthy food plan for weight loss.
Once your heel pain has improved, you will need to take these steps to prevent heel pain from returning in the future.
Acupuncture Near Me for Heel Pain
The typical treatment for heel pain can last for several months, with unpredictable results. If you have been suffering from plantar fasciitis or Achilles tendonitis, and want to heal from heel pain more quickly, it is worth it to give acupuncture a try. At Art of Wellness, we have over 30 years of experience helping patients get relief from pain conditions of all kinds. Get back on your feet again with acupuncture for heel pain!
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.