-
 Art of Wellness Acupuncture & Traditional Chinese Medicine (TCM)11704 Wilshire Blvd, Suite 295, Los Angeles, CA, 90025
Art of Wellness Acupuncture & Traditional Chinese Medicine (TCM)11704 Wilshire Blvd, Suite 295, Los Angeles, CA, 90025
myartofwellness@gmail.com310-451-5522 Office Hours
MonClosedTue7:30 am --4 pmWed7:30 am --4 pmThu7:30 am -- 4 pmFri7:30 am -- 4 pmSat7:30 am -- 4 pmSunClosedOur office opens from Tuesdays to Saturdays 7:30 am to 4 pm, will be closed on Memorial day, Independent day, Labor day, Thanksgiving day, Christmas and New year.
-
Recent Posts
- Acupuncture for Sciatica Pain
- Can Acupuncture Help With Bladder Control?
- How to Treat De Quervain’s Tenosynovitis With Acupuncture and TCM
- Chinese New Year 2026: Year of the Horse
- Acupuncture and TCM Treatment for Perimenopause Symptoms
- How to Treat Insulin Resistance With Acupuncture and TCM
- How to Treat Metabolic Syndrome With Acupuncture and TCM
- How to Treat Syncope With Acupuncture and TCM
- How to Treat Thoracic Outlet Syndrome With Acupuncture and TCM
- How to Treat Dupuytren’s Contracture With Acupuncture and TCM
- How to Treat Nutcracker Syndrome With Acupuncture and TCM
- How to Treat Rosacea With Acupuncture and TCM
- How to Treat Perioral Dermatitis With Acupuncture and TCM
- Lymphatic Drainage With Acupuncture and TCM
- How to Treat Turf Toe With Acupuncture
- How to Treat Nerve Pain With Acupuncture and TCM
- Sign up to receive news and updates and get my free report:“The Top 10 Reasons to Try Acupuncture”

February 2026 M T W T F S S 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28
What We Treat
Acupuncture for Sciatica Pain
By Qineng Tan, L.Ac., Ph.D. and Xiaomei Cai, L.Ac.
Sharp, burning pain in the buttocks that radiates down the leg? Low back pain and hip pain? These can be signs of sciatica, or nerve pain due to irritation or compression of the sciatic nerve. Acupuncture treatment can help relieve sciatic pain and promote nerve healing.
What is “sciatica?” Sciatica refers to the variety of symptoms that can arise when the sciatic nerve is irritated, due to injury, inflammation, or pinching of the nerve. These symptoms can include:
- Low back pain
- Sharp, shooting, or burning pain in the buttocks
- Nerve pain radiating down the leg
- Pain occurs with bending over or lifting legs
- Tingling or numbness, “pins and needles” sensation in the back, buttocks, leg or foot
- Muscle weakness in the leg
- “Foot drop” or dragging of foot when you walk
- In severe cases, urinary incontinence
When we say “sciatic nerve,” we are actually referring to two thick bundles of nerves that branch out of the base of the spinal cord and then run through the buttocks and down the legs. These nerves carry signals from the brain to the extremities, allowing you to make voluntary movements and communicating when there is pain or dysfunction.
Nerve pain or tingling sensations can occur at any point along the sciatic nerve bundle and tend to come and go, depending on your activity. The symptoms usually only show up on one side of the body.
Most people who experience symptoms of sciatica will find that they go away in a matter of weeks or months. In the meantime, though, sciatica pain can have a seriously negative impact on your daily life. Sciatica pain can be severe at times, affecting your motivation and ability to partake in your usual physical activities and even impacting your mental health.
Unfortunately, some people will develop chronic sciatica that can persist for months or even years. That is why it is best to address sciatic pain and not ignore it. If there are deeper problems contributing to inflammation or causing nerve damage, they need to be found and addressed.
Acupuncture treatment can help relieve sciatica pain and sensations of numbness and facilitate recovery.
What Causes Sciatica?
Sciatic nerve pain can be caused by a variety of factors or health conditions. In some cases “true sciatica” is caused by damage to or compression of the sciatic nerve. In other cases, the pain might be stemming from something else, such as piriformis syndrome, spinal disk problems, or stenosis, causing inflammation around the nerve bundle that causes pinching or compression.
Often sciatic pain develops due to improper form when lifting weight, repetitive stress from performing a task that requires bending or awkward positioning of the body, or a lack of core strength that puts too much stress on your low back when you lift something.
Some causes of sciatica include:
- Pregnancy can cause pressure on the sciatic nerve
- Osteoarthritis can damage the discs and/or cartilage in the spine
- Peripheral neuropathy related to diabetes
- Herniated disc
- Degenerative disc disease
- Spinal stenosis, or lumbar stenosis
- Bone spurs on the spine
- In rare cases, a tumor in the spine
Conventional Treatment for Sciatica

Generally, when you see your medical doctor for help with sciatic pain, the initial exam and treatment protocols will be conservative. Because imaging (x-ray, ultrasound or MRI) is not particularly helpful for showing nerve damage or impingement, typically doctors will wait to do this until the condition has gone on for more than a few months, and will be looking for herniated disks or other spinal issues.
Typical recommendations for sciatica will involve taking NSAIDs (anti-inflammatory pain medications), and using basic home remedies like cold packs and heating pads. Massage therapy may be helpful, and you might be referred to a physical therapist, who can offer some gentle exercises and stretches that may help.
If these recommendations do not help, next steps for treatment of sciatica pain may involve steroid injections or nerve root blocks, other medications, such as muscle relaxers, certain antidepressants that are known to help with nerve pain, oral corticosteroids, or opioid pain medications.
In severe, chronic cases, where the pain is related to herniated disc, spinal stenosis, or bone spurs, surgery may be suggested.
Acupuncture treatment, when used as an alternative or adjunct therapy for sciatica, can help relieve pain symptoms.
Can Acupuncture Help Sciatica?

Modern science has now been able to prove what TCM practitioners and patients have known for many centuries; acupuncture has an analgesic effect. The insertion of thin needles at specific points along the meridians can help reduce painful sensations, reduce inflammation, and help relax muscle contractions.
In fact, acupuncture is not only highly effective for the treatment of many different types of pain; it is also safer than use of pain medications, as it has no unwanted side effects.
According to TCM theory, sciatica pain is usually considered to arise due to imbalances affecting either the gallbladder (Shaoyang) meridian or the bladder (Taiyang) meridian. The presentation of pain, tingling or heaviness on one side lets the acupuncture practitioner know which meridian and system to address.
One study looked at patients who had been experiencing sciatica leg pain for at least three months due to herniated disks, but had not had surgery and were not scheduled to have surgery. Some were given ten acupuncture treatment sessions over the course of four weeks, while others were given “sham” acupuncture. (This is the control system for many studies involving acupuncture treatment.)
After two weeks, the patients who were receiving acupuncture were already reporting a significant reduction in pain and disability. At four weeks, they reported even greater improvement. At followups after 26 weeks, and a full year, the patients who had received acupuncture treatment reported continued benefits.
A systematic review of 11 clinical trials studying acupuncture treatment for sciatica found that acupuncture and acupuncture with medication were both more effective for reducing severity of pain symptoms over medication alone, and that acupuncture treatment had fewer negative side effects than taking pain medication.
Tuina massage is another TCM therapy that can help relieve low back pain or leg pain. In some cases, your acupuncture practitioner may also provide this traditional healing massage. Topical Chinese herbal analgesics, such as liniment or herbal patches may also be recommended.
Acupuncture Near Me for Sciatica in West Los Angeles
Dr. Tan and Dr. Cai of Art of Wellness Acupuncture on the Westside of Los Angeles have been treating patients for pain conditions for over 35 years. They draw upon a wealth of knowledge and experience in both Traditional Chinese Medicine and Western Medicine and are able to create an individualized treatment protocol for each patient. If you or someone you know has been suffering with low back pain, leg pain, tingling and numbness due to a pinched nerve, repetitive stress, or some other cause, please do not hesitate to reach out to Art of Wellness to schedule a consultation. Relief for sciatica pain through acupuncture treatment can help get back to your normal life again.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.
Can Acupuncture Help With Bladder Control?
By Xiaomei Cai, L.Ac., Ph.D. and Qineng Tan, L.Ac., Ph.D.
Are you struggling with urinary incontinence (UI), leaking urine, or wetting the bed at night? Acupuncture and TCM can help relieve urinary urgency and help with bladder control problems.
Bladder problems are common in people or all ages and genders, but urinary incontinence becomes more common as we get older.
Women, especially, may begin to notice changes in their urinary frequency and control as early as their 40s. Recent data suggests that 30-50% of women between the ages of 45-60 experience bladder control issues.
There are many issues that can impact bladder control:
- Nerve damage, or other nervous system-related issues
- Pregnancy trauma or trauma from pelvic surgery
- Weakness in pelvic floor muscles
- UTI – urinary tract infections
- Perimenopause and menopause changes in estrogen levels
- Enlarged prostate (BPH)
- Constipation can put pressure on the bladder
Functional Incontinence or Stress Incontinence?
Nerves are a critical part of bladder function; messages from the brain let the bladder sphincter know when it is a good time to release urine. Functional incontinence is a condition that occurs when central nervous system signals between the brain and the bladder are not linking up correctly.
“Stress incontinence” may sound like it has something to do with anxiety or emotional pressures, but in this case, the term “stress” refers to mechanical stress. When there is internal physical pressure on the bladder, from things like laughing, coughing, sneezing, or any exercise that uses the abdominal muscles, the bladder can suddenly leak.
Stress urinary incontinence is more common in women, because changes in hormones during pregnancy, childbirth, perimenopause and menopause can have a dramatic effect on the tone of the pelvic floor muscles and all of the connective tissues that keep the bladder, the urethra, and other pelvic organs in place.
Urinary Retention
While it is less common, urinary retention is also a bladder control problem. In this condition, the bladder is not completely emptying when you urinate.
Acute urinary retention occurs when there is a sudden inability to urinate, even though the bladder is clearly full. This can cause serious pain and should be addressed with a medical provider immediately.
Chronic urinary retention can begin to happen gradually over time. Signs of chronic urinary retention include:
- Having trouble when starting to urinate
- Feeling like you need to urinate again when you just went
- Feeling like you always need to urinate
- Getting up multiple times during the night to urinate
- Weak flow of urine when peeing
Urinary retention can also be caused by central nervous system issues, sagging pelvic tissues, physical obstructions like an enlarged prostate or stones in the urethra, or some medications, like muscle relaxers.
Acupuncture treatment can help with urinary incontinence and retention by working on multiple levels to positively impact the central nervous system and toning the pelvic muscles.
Typical Treatment for Bladder Control Problems

Unfortunately, many people do not seek professional help for overactive bladder symptoms or incontinence, perhaps because they feel embarrassed, they think that it’s “normal,” and/or because they aren’t aware of what types of treatment for bladder control problems are available.
Medical practitioners will often suggest lifestyle changes that may help control bladder symptoms, such as managing your intake of liquids, avoiding constipation, and losing weight.
Pelvic floor physical therapy, which seeks to strengthen the pelvic floor muscles, may also be recommended. Gentle exercises can help reduce pelvic pain and pressure, and may help reduce the sensations of urinary urgency.
For many people, these natural interventions are not enough to solve the problem. Bladder training (sometimes called “timed voiding”) by scheduling when you go to the bathroom, not drinking anything all evening, and doing Kegels at stop lights are difficult habits to maintain, especially if you’re not feeling any results.
Acupuncture treatment can help support these practices in meaningful ways, so that you will notice improvement.
In more severe cases, surgery (known as “sling surgery) may be suggested. This surgery typically involves the insertion of synthetic “mesh” to support the pelvic organs. While this helps in some cases, unfortunately, some people experience serious complications after this procedure.
Acupuncture and TCM offer an alternative treatment for urinary incontinence that can help naturally improve bladder control.
Can Acupuncture Help Incontinence?
According to TCM theory, urinary incontinence is generally considered to happen due to a weakness of the kidney Qi. Strengthening the Qi of the kidneys with acupuncture and herbs helps to improve the function of the bladder.

Urinary function depends on a complex working together of the various nervous systems within the body. The autonomic, somatic, and parasympathetic nerves are all involved in stimulating, controlling and relaxing the different muscles and sphincters that allow urine to be held and released appropriately.
While TCM views organ systems in a different way than conventional medicine does, acupuncture points have been used for centuries to influence the nervous system at the brain-body connection level, as well as to help with specific, localized muscle functioning.
Acupuncture treatment that targets specific acupoints can help reduce contraction of the bladder muscles, to prevent leaking of urine and sudden feelings of urgency.
Acupuncture also has an analgesic effect, which means it can reduce pain and related sensations. Thus, it can help relieve the physical feelings associated with urinary urgency and pelvic pressure.
This can help with the process of “bladder training,” as it may allow you to wait longer before going to the bathroom and have a clearer awareness of the bladder fully emptying when you do.
Electroacupuncture, in particular, has been shown to help reduce leakage and improve the functioning of the urethra and bladder, reducing the symptoms of stress incontinence.
Acupuncture Near Me for Bladder Control in Los Angeles
Drs. Tan and Cai at Art of Wellness Acupuncture in West Lost Angeles have over 35 years of experience helping patients with bladder issues, due to pregnancy, childbirth, perimenopause, enlarged prostate. This condition can be frustrating and embarrassing. The acupuncturists at Art of Wellness are caring and easy to talk to. They can help you feel comfortable and more confident in your daily life and sleeping through the night, without urinary problems like urgency and leaking.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.
How to Treat Thoracic Outlet Syndrome With Acupuncture and TCM
By Qineng Tan, L.Ac., Ph.D. and Xiaomei Cai, L.Ac., Ph.D.

Tingling in one arm? Stiff neck and shoulder? Neck pain or headache back of head? These can be symptoms of thoracic outlet syndrome (TOS), or compression of the nerves and blood vessels that run through the neck and shoulder. Acupuncture and TCM offer thoracic outlet treatment to help relieve pain and numbness in the arm and hand.
Tingling pain and weakness in the arm and hand are the most common signs of thoracic outlet compression syndrome. You might wake up with pins and needles in your arm, or have a feeling of weakness in your hand after lifting things overhead or working for long hours at your computer.
What Causes Thoracic Outlet Syndrome?
There is a narrow space between your top rib and your collarbone, known as the thoracic outlet, through which a complex network of nerves and vessels run, connecting the neck and shoulder to the arm.
These nerves and arteries can become constricted due to tight or misaligned muscles (particularly the scalene or pectoralis minor), poor posture, or repetitive movements at work or while participating in a sport, resulting in impaired circulation, and nerve irritation.
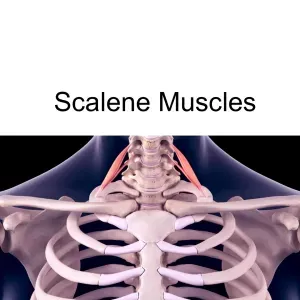
The three scalene muscles (anterior, middle, and posterior) attach the cervical vertebrae of the neck to the top two ribs. Key blood vessels (the brachial plexus, subclavian artery and vein) run through the narrow space between the scalene muscles. When these muscles become tight or pushed out of their proper alignment, this can cause compression or entrapment of the blood vessels, affecting blood flow and sometimes also putting pressure on the ulnar nerve, which extends from the neck all the way down to the hand.
Injury or trauma to the area due to a car accident (such as whiplash) could lead to thoracic outlet syndrome. Sports injuries or simply the repetitive movements involved in a sport could cause thoracic outlet syndrome to develop, particularly movements where the arm is extended above the head, as in swimming or baseball. Physical changes that occur during pregnancy and affect the posture can also aggravate nerves and blood vessels.
People with Ehlers-danlos syndrome may be more prone to developing thoracic outlet syndrome because of instability in the shoulder girdle.
In rare cases, a person might have an extra rib or other anatomical variation, which can contribute to TOS.
Top 10 Symptoms of Thoracic Outlet Syndrome
Symptoms of thoracic outlet compression syndrome can come and go and change over time. Common signs include: tingling and numbness in ring finger or pinky finger, pain in neck, pain in shoulder blade, soreness in the armpit or front of chest.
Common symptoms of thoracic outlet:
- Tingling, numbness, or a “pins and needles” sensation in the arm or hand
- Feeling of fatigue in the arm, or arm feels heavy
- Weakness in the hand grip or difficulty lifting objects, loss of fine motor skills in the hand, clumsiness, dropping things
- Aching pain or tenderness and sensitivity in the neck, shoulder, collarbone or chest, sometimes radiating down the arm
- Shoulder appears to be drooping, slumped posture
- Swelling, discoloration, and/or a sensation of cold in the affected arm or hand
- Headaches, especially pain in the back of the head, headache at the base of the skull
- Loss of muscle in the base of the thumb
- Weak pulse in the affected arm
- Blood clots or deep vein thrombosis
Symptoms like tingling and weakness of the arm and hand usually become worse after the arm has been in an elevated position, performing activities that require the arm to be raised over the head.
Signs of thoracic outlet syndrome can appear similar to those of other conditions, like carpal tunnel syndrome, cubital tunnel syndrome, cervical radiculopathy, or other cervical spine issues. Some of the symptoms of thoracic outlet syndrome are also similar to the symptoms of a heart attack.
Typical Thoracic Outlet Syndrome Therapies
Diagnosis of TOS generally begins with a detailed medical history and physical exam, in which maneuvering the arm or neck rotation may reproduce symptoms. Imaging tests such as X-rays, MRI, CT scans, or Doppler ultrasound help assess anatomical contributors and vascular involvement. Nerve conduction studies can also confirm nerve compression.
Conventional treatment for thoracic outlet syndrome typically starts conservatively. A central focus is on physical therapy, aimed at stretching tight muscles, improving posture, and strengthening supportive muscle groups. Pain may be managed with medications like NSAIDs or muscle relaxants. If symptoms persist or worsen, interventions such as targeted injections (e.g., botulinum toxin into tight scalene muscles) or surgical options (like first-rib resection) may be suggested.
These methods can offer relief, especially when implemented early. Still, recovery can be prolonged and some patients may experience recurring symptoms. Acupuncture and TCM offer alternative management for thoracic outlet syndrome.
Can Acupuncture Help Thoracic Outlet Syndrome?

In Traditional Chinese Medicine, thoracic outlet syndrome is viewed as a problem of Qi (energy) and blood stagnation within the meridians that traverse the neck and shoulders, especially the Liver, Gallbladder, and Lung channels. Emotional stress, poor posture, or physical strain may disrupt the smooth flow of Qi, leading to obstructions that manifest as pain, numbness, or movement difficulty.
Additional contributing factors may include Wind-Cold-Damp invasion, which contracts muscles; Liver Qi stagnation, which impairs flexibility; and Spleen or Kidney weakness, which fails to support the body’s structural integrity and recovery.
TCM addresses both the symptomatic blockage and the deeper systemic imbalances underlying the condition.
TCM Treatment for Thoracic Outlet Syndrome
TCM takes a multi-dimensional approach to treating TOS. Acupuncture uses fine needles to stimulate key points that encourage the release of stagnant Qi and improve blood flow.
Cupping and Gua Sha techniques help soften fascia, reduce muscle tension, and encourage lymphatic and blood circulation.
Herbal formulas may include herbs that invigorate blood, relax sinews, and strengthen muscles and fascia.
Lifestyle changes, emphasizing improved posture, ergonomic adjustments, mindful movement, stress management, and dietary tips can help reduce inflammation and support healing.
Controlled trials and case studies suggest acupuncture effectively reduces pain and improves function in conditions involving neurovascular compression. For instance, a controlled study published in 2019 reported significant decreases in pain and disability among patients receiving acupuncture for TOS symptoms.
Another case study found that acupuncture combined with TCM herbal therapy provided thoracic outlet syndrome relief by alleviating shoulder tightness, restoring flexibility, and reducing numbness.
Several clinical groups are exploring acupuncture-mediated modulation of microcirculation, inflammatory markers, and nerve conduction—underscoring its role as a promising complement to standard care.
Acupuncture Near Me for Thoracic Outlet Syndrome in West Los Angeles
TCM modalities are excellent for helping to relieve pain and tingling and improving range of motion for a wide variety of conditions. Acupuncture can provide symptom relief and fundamental improvement of conditions like nutcracker syndrome, carpal tunnel syndrome, cubital tunnel, syndrome, nerve pain, shoulder pain, neck pain, and thoracic outlet syndrome. Drs. Tan and Cai at Art of Wellness in Santa Monica/West Los Angeles have over 35 years of experience in treating vascular and nerve conditions.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.
How to Treat Dupuytren’s Contracture With Acupuncture and TCM
By Qineng Tan, L.Ac., Ph.D. and Xiaomei Cal, L.Ac., Ph.D.

Fingers bent and can’t straighten? Dupuytren’s contracture is a condition in which the tissues under the skin of the fingers get thick and tight, making it hard to open your hand fully. Acupuncture and TCM offer alternative treatment for Dupuytren’s Contracture to help improve mobility in the fingers and hand.
Dupuytren’s Contracture is a progressive condition that causes the fingers—most often the ring and pinky fingers—to bend toward the palm, eventually interfering with hand function. Although it often develops slowly over several years, the impact on everyday activities can be significant.
What Is Dupuytren’s Contracture?
Dupuytren’s Contracture is a connective tissue disorder that affects the palmar fascia—the fibrous layer beneath the skin of the palm and fingers. Over time, this tissue thickens and shortens into tough, cord-like structures that gradually pull the fingers into a bent position.
This condition most commonly affects the ring and pinky fingers. While the condition is typically painless, it can significantly limit hand function, making it difficult to perform daily tasks like grasping objects, typing, or even shaking hands.
It is more common in older adults, particularly men, and often develops in both hands, though one may be more severely affected. Patients may also notice small nodules or puckering of the skin in the palm during the early stages.
Symptoms of Dupuytren’s Contracture
In the beginning, the condition might present as a small lump or thickened band of tissue in the palm. These fibrous cords become more pronounced over time, leading to increasing difficulty in extending one or more fingers.
Typically, the ring and little fingers are affected. As the disease progresses, the fingers are pulled inward toward the palm in a flexed position. This flexion limits hand mobility and can make everyday tasks, such as putting hands in pockets or wearing gloves, challenging. Additionally, the skin on the palm may appear puckered or dimpled, reflecting the tightening of the underlying fascia.
Top 5 Signs of Dupuytren’s Contracture
- A small lump or nodule in the palm or thickened bands or cords of tissue under the skin
- Difficulty fully extending one or more fingers
- Fingers (typically ring and pinky) pulled into a bent position
- Loss of hand function or reduced range of motion
- Puckering or dimpling of the skin on the palm
In the early stages, symptoms of Dupuytren’s Contracture may be subtle and not interfere much with hand use. As the contracture progresses, everyday tasks can become increasingly difficult.
What Causes Dupuytren’s Contracture?

Although the exact cause remains unknown, several risk factors are known to contribute to the development of Dupuytren’s Contracture. Genetics seem to play a significant role; people with a family history of the condition are at a higher risk of developing the condition.
Certain health conditions, such as diabetes and epilepsy, have been linked to a higher incidence of Dupuytren’s. Lifestyle choices like smoking and heavy alcohol use may also contribute to the formation of these fibrous hand contractures by promoting inflammation and poor circulation.
Conventional Diagnosis and Treatment for Dupuytren’s Contracture
A medical diagnosis of Dupuytren’s Contracture typically involves a physical examination and a discussion of symptoms. One common clinical assessment is the “tabletop test,” in which the patient tries to lay their hand flat on a surface. Inability to do so often indicates the presence of contracture.
In early or mild cases where the fingers are still mostly functional, doctors may suggest observation. However, if the condition progresses to the point where hand function is compromised, treatment becomes necessary.
Conventional treatments include steroid injections to reduce inflammation in nodules, enzyme injections such as collagenase to weaken the cords and allow manual extension, and needle aponeurotomy, a technique that involves breaking up the thickened tissue with a needle. In more advanced cases, surgical removal of the diseased fascia, known as fasciectomy, may be required. Though these interventions can be effective in the short term, recurrence is common, and recovery—particularly from surgery—can be long and uncomfortable.
Can Acupuncture Help Dupuytren’s Contracture?
In Traditional Chinese Medicine, Dupuytren’s Contracture is seen as a manifestation of internal imbalances that obstruct the flow of Qi and blood through the meridians of the hand. The condition corresponds with what TCM describes as “Bi syndrome,” or painful obstruction syndrome. According to TCM theory, this condition often arises from external pathogenic factors like Wind, Cold, and Dampness invading the meridians and causing stagnation. Over time, this stagnation leads to blood stasis and the formation of hard nodules and fibrous bands that contract the hand.
Additionally, internal imbalances—such as Liver Qi stagnation, which impairs the smooth flow of energy and affects the sinews, and Kidney deficiency, which weakens the bones and tendons—may underlie the development of this condition. These factors contribute to the gradual stiffening and deformity of the hand over time.
A TCM approach to treating Dupuytren’s Contracture focuses on restoring the proper flow of Qi and blood, relaxing tendons, and softening nodules. Acupuncture can help increase circulation, reduce inflammation, and relieve the tightness and rigidity in the fascia. Local needling around the palm and forearm is often combined with other points along the meridians to address systemic imbalances.
Moxibustion, the therapeutic application of heat using the dried herb mugwort, is sometimes applied over the affected area to dispel Cold and Dampness and improve local blood flow. This can help relieve stiffness and improve finger mobility. Tui Na, or Chinese medical massage, may also be used to manipulate the hand and fingers, helping to break up fibrous tissue and restore range of motion.
Herbal medicine—both internal formulas and topical liniments—can be customized to nourish the blood, dispel stasis, and promote tendon health.
Cupping therapy may also be incorporated to stimulate circulation and relax the contracted fascia. These methods, used together, provide a comprehensive, non-invasive way to manage symptoms and potentially slow the progression of Dupuytren’s Contracture.
One case study reported significant improvements in a patient’s hand mobility, along with reduced pain and thickening of tissue, after a series of six acupuncture treatments supported by moxibustion and herbal therapy.
Another published case study described how acupuncture and electroacupuncture helped a patient reduce the thickness of nodules and regain finger extension.
Research into acupuncture’s effectiveness in treating fibrotic and musculoskeletal disorders suggests that this modality may be especially well-suited for managing connective tissue issues. Acupuncture can promote fibroblast remodeling, modulate inflammation, and improve microcirculation—mechanisms that are directly relevant to the treatment of Dupuytren’s.
Acupuncture Near Me for Dupuytren’s Contracture in West Los Angeles
If you’re noticing a thickening in your palm or your fingers are beginning to curl inward, you don’t have to wait until surgery becomes necessary. Early intervention with acupuncture and Traditional Chinese Medicine may help restore mobility, reduce discomfort, and potentially slow the progression of Dupuytren’s Contracture.
At Art of Wellness Acupuncture in West Los Angeles, we create personalized treatment plans that address the whole person—targeting both symptoms and the root imbalances underlying them. Contact us today to learn how we can help you regain full use of your hands with the help of TCM.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.
How to Treat Perioral Dermatitis With Acupuncture and TCM
By Xiaomei Cai, L.Ac., Ph.D. and Qineng Tan, L.Ac.

Itchy red bumps around mouth, nose, or under eyes? Perioral dermatitis is a common inflammatory skin condition that shows up as a red, bumpy rash on the face. Acupuncture and TCM offers a holistic way to help get rid of perioral dermatitis.
What Is Perioral Dermatitis?
Perioral dermatitis is a type of face rash that primarily affects the area around the mouth (perioral), though it can also show up around the nose (perinasal dermatitis) and eyes (periorbital dermatitis). This condition is most commonly seen in women aged 20–45, but it can affect men and children as well. It’s considered a form of rosacea or a rosacea-like condition by many dermatologists, though it has its own distinct features.
Unlike acne, the red bumps in perioral dermatitis don’t contain pus, and unlike eczema, the rash is not typically scaly or flaky. It often appears suddenly and can be persistent, sometimes lasting for weeks or months.
Traditional Chinese Medicine (TCM), including acupuncture and herbal therapy, offers a natural approach to different types of dermatitis that focuses on healing the skin and addressing underlying imbalances that cause this condition.
Top 5 Symptoms of Perioral Dermatitis

Perioral dermatitis can sometimes be mistaken for other health issues that cause skin rashes or other skin conditions, such as: acne, herpes, rosacea, contact dermatitis, seborrheic dermatitis, discoid lupus, and papula sarcoidoisi. The most common signs of Perioral Dermatitis include:
- Red, inflamed bumps around the mouth, nose, or eyes
- Burning or itching sensation in the affected area
- Dry, tight, or peeling skin
- Clear fluid or pus in some bumps (though usually not like acne)
- Rash that spares the skin directly around the lips (creating a clear border)
Typically, perioral dermatitis will become worse with use of corticosteroid creams or heavy moisturizers.
It is important to recognize this condition, so that it can be treated appropriately.
What Causes Perioral Dermatitis?
The exact cause of perioral dermatitis is not fully understood, but several triggers and contributing factors have been identified. People who already suffer from eczema may be more prone to developing perioral dermatitis, because eczema can affect the skin barrier. Here are some of the things that might trigger an perioral dermatitis outbreak or flare up:
Topical corticosteroid use – This is the most common trigger. Long-term use of steroid creams, even over-the-counter hydrocortisone, can lead to this rash.
Hormonal changes – Many people who menstruate notice flare-ups around their menstrual cycle or during times of hormonal fluctuation.
Use of heavy facial creams or cosmetics – Occlusive skin products may block pores and irritate the skin.
Fluoridated toothpaste – Some people find their symptoms worsen with fluoride-containing toothpaste.
Environmental triggers – Sun exposure, wind, and heat can aggravate the skin.
Microbial imbalance – Overgrowth of certain bacteria or yeast on the skin may play a role.
Stress – Emotional stress can weaken the immune system and disrupt skin balance.
Dietary factors – Some people report flares related to certain foods, like spicy foods or alcohol.
Diagnosis and Treatment for Perioral Dermatitis
In a conventional medical setting, diagnosis is typically made based on a visual exam and patient history. A dermatologist may ask about what kinds of skincare products you use, medications (especially steroid use), and recent lifestyle changes.
Standard treatments include:
Discontinuation of steroid creams – Although this may cause a rebound flare, it is essential to stop steroid use.
Topical antibiotics or anti-inflammatory creams – Such as metronidazole or clindamycin.
Oral antibiotics – Like tetracycline or doxycycline, especially for more stubborn cases.
Skin care guidance – Patients are usually advised to stop all current products and switch to a minimalist routine with gentle cleansers and no makeup.
While these treatments can be effective, they don’t always address the root cause, and relapses are common—especially if underlying imbalances are not corrected.
TCM for Perioral Dermatitis

Traditional Chinese Medicine sees perioral dermatitis not just as a skin problem, but as a sign of deeper internal disharmony. In TCM, the health of the skin is closely related to the health of the Lung, Stomach, and Spleen organ systems. When there is heat, dampness, or toxicity trapped in the body, it can manifest as inflammation on the skin.
For example, a rash around the mouth is often related to Stomach Heat or Spleen Dampness, especially if digestion is weak or the diet is rich in spicy or greasy foods. If the rash appears around the nose and cheeks, Lung Heat or Wind-Heat may be contributing factors.
TCM also considers emotional stress and hormonal imbalance as key factors in skin conditions. Emotional stress can create stagnation in the Liver system, while hormonal changes may disrupt the balance of Yin and Yang in the body, leading to heat and inflammation.
Can Acupuncture Help Perioral Dermatitis?
Acupuncture and TCM therapies aim to treat the root cause of perioral dermatitis while also calming the skin and promoting healing.
Acupuncture helps regulate the immune system, reduce inflammation, and rebalance the organ systems involved. Specific acupuncture points may be used to clear heat, drain dampness, and support the Spleen and Lung.
Chinese herbal medicine can be customized to each patient’s individual pattern. Herbal formulas will be customized for each individual, depending on the presentation.
Dietary and lifestyle recommendations are often part of treatment, helping patients avoid inflammatory foods, support digestion, and reduce stress.
Facial gua sha and herbal washes can be used as topical therapies to calm redness, promote lymphatic drainage, and soothe irritated skin.
In many cases, patients find that their rash improves significantly with a few weeks of consistent acupuncture and herbal therapy—without the side effects of antibiotics or topical steroids.
While studies specifically on acupuncture for perioral dermatitis are limited, research shows that acupuncture is effective in treating other inflammatory skin conditions like eczema, acne, and rosacea. These studies demonstrate that acupuncture can reduce inflammation, balance hormones, and modulate the immune system, which are all key factors in healing perioral dermatitis.
A review found that acupuncture reduced itch, redness, and lesion count in patients with atopic dermatitis. Another study noted improvement in acne symptoms with acupuncture and herbal medicine, especially in women with hormonal imbalances.
Acupuncture Near Me for Perioral Dermatitis in West Los Angeles
If you’ve been struggling with persistent or recurring perioral dermatitis and are looking for a more holistic, drug-free way to manage your symptoms, acupuncture and Traditional Chinese Medicine offer a safe and effective alternative. By treating both the surface symptoms and the internal imbalances, we help the skin heal from the inside out.
At Art of Wellness Acupuncture, we specialize in treating chronic skin conditions like perioral dermatitis using the principles of Traditional Chinese Medicine. Every treatment is tailored to your unique constitution and lifestyle, so you can heal naturally and prevent future flare-ups. If you’re dealing with red, itchy bumps around your mouth or face, don’t wait—reach out today to schedule your consultation and get started on the path to clearer, calmer skin.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.