-
 Art of Wellness Acupuncture & Traditional Chinese Medicine (TCM)11704 Wilshire Blvd, Suite 295, Los Angeles, CA, 90025
Art of Wellness Acupuncture & Traditional Chinese Medicine (TCM)11704 Wilshire Blvd, Suite 295, Los Angeles, CA, 90025
myartofwellness@gmail.com310-451-5522 Office Hours
MonClosedTue7:30 am --4 pmWed7:30 am --4 pmThu7:30 am -- 4 pmFri7:30 am -- 4 pmSat7:30 am -- 4 pmSunClosedOur office opens from Tuesdays to Saturdays 7:30 am to 4 pm, will be closed on Memorial day, Independent day, Labor day, Thanksgiving day, Christmas and New year.
-
Recent Posts
- Can Acupuncture Help With Bladder Control?
- How to Treat De Quervain’s Tenosynovitis With Acupuncture and TCM
- Chinese New Year 2026: Year of the Horse
- Acupuncture and TCM Treatment for Perimenopause Symptoms
- How to Treat Insulin Resistance With Acupuncture and TCM
- How to Treat Metabolic Syndrome With Acupuncture and TCM
- How to Treat Syncope With Acupuncture and TCM
- How to Treat Thoracic Outlet Syndrome With Acupuncture and TCM
- How to Treat Dupuytren’s Contracture With Acupuncture and TCM
- How to Treat Nutcracker Syndrome With Acupuncture and TCM
- How to Treat Rosacea With Acupuncture and TCM
- How to Treat Perioral Dermatitis With Acupuncture and TCM
- Lymphatic Drainage With Acupuncture and TCM
- How to Treat Turf Toe With Acupuncture
- How to Treat Nerve Pain With Acupuncture and TCM
- How to Treat Watery Eyes With Acupuncture and TCM
- Sign up to receive news and updates and get my free report:“The Top 10 Reasons to Try Acupuncture”

January 2026 M T W T F S S 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31
Cupping
How to Treat Dupuytren’s Contracture With Acupuncture and TCM
By Qineng Tan, L.Ac., Ph.D. and Xiaomei Cal, L.Ac., Ph.D.

Fingers bent and can’t straighten? Dupuytren’s contracture is a condition in which the tissues under the skin of the fingers get thick and tight, making it hard to open your hand fully. Acupuncture and TCM offer alternative treatment for Dupuytren’s Contracture to help improve mobility in the fingers and hand.
Dupuytren’s Contracture is a progressive condition that causes the fingers—most often the ring and pinky fingers—to bend toward the palm, eventually interfering with hand function. Although it often develops slowly over several years, the impact on everyday activities can be significant.
What Is Dupuytren’s Contracture?
Dupuytren’s Contracture is a connective tissue disorder that affects the palmar fascia—the fibrous layer beneath the skin of the palm and fingers. Over time, this tissue thickens and shortens into tough, cord-like structures that gradually pull the fingers into a bent position.
This condition most commonly affects the ring and pinky fingers. While the condition is typically painless, it can significantly limit hand function, making it difficult to perform daily tasks like grasping objects, typing, or even shaking hands.
It is more common in older adults, particularly men, and often develops in both hands, though one may be more severely affected. Patients may also notice small nodules or puckering of the skin in the palm during the early stages.
Symptoms of Dupuytren’s Contracture
In the beginning, the condition might present as a small lump or thickened band of tissue in the palm. These fibrous cords become more pronounced over time, leading to increasing difficulty in extending one or more fingers.
Typically, the ring and little fingers are affected. As the disease progresses, the fingers are pulled inward toward the palm in a flexed position. This flexion limits hand mobility and can make everyday tasks, such as putting hands in pockets or wearing gloves, challenging. Additionally, the skin on the palm may appear puckered or dimpled, reflecting the tightening of the underlying fascia.
Top 5 Signs of Dupuytren’s Contracture
- A small lump or nodule in the palm or thickened bands or cords of tissue under the skin
- Difficulty fully extending one or more fingers
- Fingers (typically ring and pinky) pulled into a bent position
- Loss of hand function or reduced range of motion
- Puckering or dimpling of the skin on the palm
In the early stages, symptoms of Dupuytren’s Contracture may be subtle and not interfere much with hand use. As the contracture progresses, everyday tasks can become increasingly difficult.
What Causes Dupuytren’s Contracture?

Although the exact cause remains unknown, several risk factors are known to contribute to the development of Dupuytren’s Contracture. Genetics seem to play a significant role; people with a family history of the condition are at a higher risk of developing the condition.
Certain health conditions, such as diabetes and epilepsy, have been linked to a higher incidence of Dupuytren’s. Lifestyle choices like smoking and heavy alcohol use may also contribute to the formation of these fibrous hand contractures by promoting inflammation and poor circulation.
Conventional Diagnosis and Treatment for Dupuytren’s Contracture
A medical diagnosis of Dupuytren’s Contracture typically involves a physical examination and a discussion of symptoms. One common clinical assessment is the “tabletop test,” in which the patient tries to lay their hand flat on a surface. Inability to do so often indicates the presence of contracture.
In early or mild cases where the fingers are still mostly functional, doctors may suggest observation. However, if the condition progresses to the point where hand function is compromised, treatment becomes necessary.
Conventional treatments include steroid injections to reduce inflammation in nodules, enzyme injections such as collagenase to weaken the cords and allow manual extension, and needle aponeurotomy, a technique that involves breaking up the thickened tissue with a needle. In more advanced cases, surgical removal of the diseased fascia, known as fasciectomy, may be required. Though these interventions can be effective in the short term, recurrence is common, and recovery—particularly from surgery—can be long and uncomfortable.
Can Acupuncture Help Dupuytren’s Contracture?
In Traditional Chinese Medicine, Dupuytren’s Contracture is seen as a manifestation of internal imbalances that obstruct the flow of Qi and blood through the meridians of the hand. The condition corresponds with what TCM describes as “Bi syndrome,” or painful obstruction syndrome. According to TCM theory, this condition often arises from external pathogenic factors like Wind, Cold, and Dampness invading the meridians and causing stagnation. Over time, this stagnation leads to blood stasis and the formation of hard nodules and fibrous bands that contract the hand.
Additionally, internal imbalances—such as Liver Qi stagnation, which impairs the smooth flow of energy and affects the sinews, and Kidney deficiency, which weakens the bones and tendons—may underlie the development of this condition. These factors contribute to the gradual stiffening and deformity of the hand over time.
A TCM approach to treating Dupuytren’s Contracture focuses on restoring the proper flow of Qi and blood, relaxing tendons, and softening nodules. Acupuncture can help increase circulation, reduce inflammation, and relieve the tightness and rigidity in the fascia. Local needling around the palm and forearm is often combined with other points along the meridians to address systemic imbalances.
Moxibustion, the therapeutic application of heat using the dried herb mugwort, is sometimes applied over the affected area to dispel Cold and Dampness and improve local blood flow. This can help relieve stiffness and improve finger mobility. Tui Na, or Chinese medical massage, may also be used to manipulate the hand and fingers, helping to break up fibrous tissue and restore range of motion.
Herbal medicine—both internal formulas and topical liniments—can be customized to nourish the blood, dispel stasis, and promote tendon health.
Cupping therapy may also be incorporated to stimulate circulation and relax the contracted fascia. These methods, used together, provide a comprehensive, non-invasive way to manage symptoms and potentially slow the progression of Dupuytren’s Contracture.
One case study reported significant improvements in a patient’s hand mobility, along with reduced pain and thickening of tissue, after a series of six acupuncture treatments supported by moxibustion and herbal therapy.
Another published case study described how acupuncture and electroacupuncture helped a patient reduce the thickness of nodules and regain finger extension.
Research into acupuncture’s effectiveness in treating fibrotic and musculoskeletal disorders suggests that this modality may be especially well-suited for managing connective tissue issues. Acupuncture can promote fibroblast remodeling, modulate inflammation, and improve microcirculation—mechanisms that are directly relevant to the treatment of Dupuytren’s.
Acupuncture Near Me for Dupuytren’s Contracture in West Los Angeles
If you’re noticing a thickening in your palm or your fingers are beginning to curl inward, you don’t have to wait until surgery becomes necessary. Early intervention with acupuncture and Traditional Chinese Medicine may help restore mobility, reduce discomfort, and potentially slow the progression of Dupuytren’s Contracture.
At Art of Wellness Acupuncture in West Los Angeles, we create personalized treatment plans that address the whole person—targeting both symptoms and the root imbalances underlying them. Contact us today to learn how we can help you regain full use of your hands with the help of TCM.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.
How to Treat Myofascial Pain Syndrome With Acupuncture and TCM
By Xiaomei Cai, L.Ac., Ph.D. and Qineng Tan, L.Ac., Ph.D.

Muscle aches and pains? Knotted muscles? Pain in trigger points? These could be signs of myofascial pain syndrome. Acupuncture and TCM can provide myofascial release and help relieve chronic myofascial pain (MPS pain).
Myofascial pain disorder is a common, yet often overlooked chronic pain condition that affects the muscles and fascia. Fascia is the thin connective tissue that is found all over the body, holding muscles, organs, and blood vessels together. Fascia is also filled with nerves, which makes it highly sensitive.
Healthy fascia is thin, stretchy and pliable. Stress, injuries, weakness and other issues can cause fascia to tighten up, become sticky, dry, or thicker. This can cause painful knots to develop in your muscles.
These areas are sometimes called fascial adhesions, or myofascial trigger points, and they can be very tender to the touch and cause muscle soreness, aches and pains.
Chronic myofascial pain can seem very similar to fibromyalgia, or symptoms of ME/CFS, and is sometimes misdiagnosed as such. However, these conditions are distinct from one another.
Fibromyalgia causes widespread, diffuse pain and tenderness all over the body, while myofascial pain is centered around specific trigger point sites. Fibro, as it is sometimes called, is believed to be caused by a disorder within the central nervous system. Fibromyalgia is usually triggered by stress, trauma, hormonal changes, lack of sleep, or sensitivities to weather changes.
It has been suggested that long-term myofascial pain syndrome may ultimately lead to a person developing fibromyalgia, as the brain and nervous system become so used to experiencing pain that they begin to produce disordered pain signaling.
Acupuncture treatment, cupping, and therapeutic Chinese massage can provide trigger point therapy that is effective for relieving tight muscles and soreness.
Myofascial Pain Syndrome Symptoms

People experience myofascial pain differently from one another; each case is unique. For some people, the pain can come and go suddenly; for others, it’s a constant, dull pain.
Myofascial pain syndrome can feel like:
- Tight muscles, stiffness
- Throbbing pain
- Dull, aching pain
- Sore muscles, tender areas
- Knotted muscles, nodules or bumps in specific areas that are sore
- Muscle weakness
- Limited range of motion
- Trouble sleeping
- Headaches
- Fatigue
Myofascial pain can be localized in one area, or referred pain, which spreads to other nearby areas. Myofascial referred pain patterns can look like pain that originates in the rotator cuff which then spreads to the deltoid, and even down the arm to the hand.
What Causes Myofascial Pain?
Medical science is not entirely clear on the causes of myofascial pain syndrome, but it seems to occur more often in people who have experienced things like:
- Periods of inactivity, such as having one of your limbs in a cast
- Repetitive movements in your work
- Pinched nerves
- Injury to a muscle or muscle group
- Having to work outdoors in the cold
- Diabetic neuropathy
- Thyroid disorders, hypothyroidism
- Deficiencies in Vitamin D or folate, or iron deficiency
- Stress, chronic tension that leads to clenched muscles
- Structural conditions like scoliosis, spondylosis, or osteoarthritis
Estimates suggest that the majority of people who are treated for chronic musculoskeletal pain may have myofascial pain syndrome. Up to 85% of the general population may experience myofascial pain at some point in time.
Treatment for Myofascial Pain Syndrome
One of the primary approaches to managing myofascial pain syndrome is physical therapy. Physical therapists may use manual therapy, stretching exercises, and postural correction to address muscle imbalances, improve flexibility, and release tension in affected muscles. Trigger point therapy, which involves applying pressure to trigger points to release muscle knots and promote relaxation, is a common component of physical therapy for MPS.
Modalities such as heat therapy and cold therapy may also be used in conjunction with physical therapy to provide pain relief and enhance the effectiveness of treatment. Heat therapy helps to increase blood flow and promote muscle relaxation, while cold therapy can reduce inflammation and numb the affected area.
In addition to physical therapy and modalities, medications may be prescribed to manage pain and improve symptoms associated with myofascial pain syndrome. Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen may be recommended to reduce inflammation and alleviate pain. Muscle relaxants such as cyclobenzaprine or benzodiazepines may also be prescribed to help relax tense muscles and improve sleep quality. In some cases, tricyclic antidepressants or anticonvulsant medications may be used to modulate pain signals and improve overall pain management.
Trigger point injections are another treatment option for myofascial pain syndrome, particularly for individuals who experience severe or persistent symptoms that do not respond adequately to conservative measures. During a trigger point injection procedure, a local anesthetic or corticosteroid is injected directly into the trigger point to help alleviate pain and reduce muscle tension.
Acupuncture needling is also considered an effective and valuable treatment option for myofascial release and relief of musculoskeletal pain.
Can Acupuncture Help Myofascial Pain Syndrome?

Many studies conducted over the past two decades point to acupuncture as an effective mode of treatment for myofascial pain syndrome.
Acupuncture is effective for myofascial pain because it can positively affect the central nervous system, increase blood flow, increase endorphin production, improve fascial adhesions, and promote muscle relaxation. Acupoints used in TCM correspond closely with myofascial trigger points.
One study looked at patients who received two acupuncture treatments per week for four weeks on trigger points in the upper trapezius. Patients reported significant reduction in pain after just two weeks.
Another study followed two groups of patients with myofascial pain centered in the neck area. One group received acupuncture treatment. The other group had acupuncture and also engaged in regular aerobic exercise. Findings showed that both groups experienced significant improvement in pain symptoms.
A review of studies found that acupuncture was effective both for reducing myofascial pain and improving function and mobility.
Acupuncturists may also use electro-acupuncture, cupping, and massage techniques like gua sha and tui na to help move lymph and blood, release muscle trigger points, and improve muscular movement that has been limited by pain.
Acupuncture Near Me for Myofascial Pain Syndrome in Los Angeles
At Art of Wellness Acupuncture in West L.A., we have over 35 years of experience helping people find relief from musculoskeletal pain of all kinds. Dr. Tan and Dr. Cai are able to use electro-acupuncture, cupping, and massage techniques like Tuina for myofascial release. If you are suffering from muscle pain and tenderness, do not hesitate to make an appointment with us.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.
How to Treat Ankylosing Spondylitis With Acupuncture and TCM
By Qineng Tan, L.Ac., Ph.D. and Xiaomei Cai, L.Ac., Ph.D.
Low back pain, morning stiffness, hip pain? Fatigue, losing weight, poor vision, skin rashes? These can all be signs of Ankylosing Spondylitis (AS). Ankylosing Spondylitis is a type of autoimmune arthritis. Acupuncture can help relieve Ankylosing Spondylitis symptoms like lower back pain.
Ankylosing spondylitis is a chronic inflammatory arthritis condition that most often affects the spine, usually the lower back and pelvis is an inflammatory disease; the primary symptom is inflammation in the sacroiliac joints, the joints where the base of the spine (the ilium) meets the pelvis (the sacrum).
Similar to rheumatoid arthritis (RA), ankylosing spondylitis is an arthritic condition triggered by a person’s immune system mistakenly attacking healthy tissues. Arthritis generally refers to pain and swelling in joint tissues.
Ankylosing spondylitis can also affect the hips, knees, shoulder joints, and/or the ribcage. When the body tries to heal affected bones, extra bone tissue begins to grow. This new bone growth is what causes joint stiffness and lack of flexibility. When the ribs are affected, it can restrict normal breathing.
Ankylosing spondylitis can, over time, weaken bones to the extent that they begin to collapse; these compression fractures can ultimately lead to curvature of the spine and a stooped posture. These fractures of the vertebrae can potentially affect the spinal cord and nerves.
“Ankylosis” is a term for the stiffening and fusion of bones. A “fused spine” can be the eventual outcome of Ankylosing spondylitis.
AS can also cause inflammation in the GI tract, causing gastrointestinal symptoms like diarrhea. In this sense, it is a type of inflammatory bowel disease (IBD).
In some cases, ankylosing spondylitis can cause eye inflammation, leading to vision problems like blurred vision, sensitivity to light, and painful eyes.
AS can also cause inflammation in the heart, which affects the function of the aortic valve and increases risk of heart disease.
As with other autoimmune disorders, modern medicine research has yet to discover what causes Ankylosing Spondylitis. Some gene mutations have been linked to ankylosing spondylitis, which is sometimes called axial spondyloarthritis.
Medical treatment for ankylosing spondylitis helps manage symptoms and slow the progression of the disease.
Acupuncture is widely recognized as an effective adjunct treatment for ankylosing spondylitis that can help reduce pain and improve mobility.
Top 10 Ankylosing Spondylitis Symptoms

The initial onset of symptoms of ankylosing spondylitis often includes episodes of lower back pain and stiffness or hip pain, which then may get more severe over time. But symptoms can vary widely from person to person, depending on which parts of the body are affected.
Symptoms of Ankylosing Spondylitis include:
- Persistent lower back pain and stiffness, typically worse in the morning and after periods of inactivity; back pain that improves with movement and exercise
- Pain and stiffness that radiate from the lower back to the buttocks, hips, and thighs, reduced flexibility and range of motion in the spine
- Hip pain, shoulder pain, chest pain, rib pain, knee pain, and/or ankle pain
- Difficulty taking deep breaths due to stiffness in the chest and ribcage
- Fatigue
- Bony fusion of vertebrae, leading to a stooped posture and loss of spinal mobility
- Eye inflammation (uveitis) causes eye pain, sensitivity to light, and blurred vision
- Loss of appetite, weight loss
- Psoriasis, skin rash
- Abdominal pain, diarrhea
There is usually a gradual progression of AS symptoms over time, potentially leading to severe spinal deformity and disability.
Conventional treatment, with acupuncture and TCM used as a complementary treatment, can be helpful for symptomatic relief.
Ankylosing Spondylitis Treatment
While there is no cure for AS, conventional medical treatments aim to manage symptoms, prevent complications, and improve quality of life for individuals with the condition.
NSAIDs such as ibuprofen, naproxen, and celecoxib are commonly used to reduce pain and inflammation associated with AS. They can help relieve symptoms and improve mobility, particularly during flare-ups.
Disease-Modifying Antirheumatic Drugs (DMARDs) like sulfasalazine and methotrexate may be prescribed to slow the progression of AS and reduce inflammation. These medications work by suppressing the immune system’s abnormal response, which contributes to inflammation, the formation of extra bone tissue, and damage to the joints.
Biologic drugs, such as tumor necrosis factor (TNF) inhibitors like adalimumab, etanercept, and infliximab, target specific components of the immune system involved in inflammation. They are often prescribed for individuals with moderate to severe AS who do not respond adequately to NSAIDs or DMARDs.
Physical therapy can play a crucial role in the management of AS by helping to improve flexibility, posture, and range of motion. Exercise programs tailored to the individual’s needs can help strengthen muscles, reduce pain, and maintain spinal mobility.
Orthopedic interventions, such as braces and orthotics, may be recommended to support proper posture and prevent spinal deformities caused by AS. In severe cases, surgical procedures like spinal fusion may be considered to stabilize the spine and alleviate pain.
Individuals with AS require regular monitoring by healthcare providers to assess disease activity, monitor medication effectiveness, and detect any complications early. Adjustments to treatment plans may be necessary based on disease progression and individual response to therapy.
Can Acupuncture Help Ankylosing Spondylitis?

Acupuncture and moxibustion have been used for centuries to help relieve joint pain and stiffness due to inflammation. In Chinese, conditions that might involve bone fusion are called “zhu jie yang,” which means “bamboo spine.”
According to TCM theory, the bones are nourished by the kidney system; we observe that the formation of AS symptoms occurs along the Kidney Meridian and the Governing Vessel meridian. Weakness in bones may be due to deficiency of kidney Qi and blockage of the Governing Vessel.
Painful areas arise when there are blockages in Qi. Blockages occur due to pathogenic forces of phlegm accumulation, cold, and dampness.
Acupuncture treatment, herbs, and moxibustion may be used to strengthen the kidneys, address kidney yang deficiency, and clear dampness and wind from the channels.
One study found that patients who were diagnosed with ankylosing spondylitis and kidney yang deficiency and were given acupuncture treatment and moxibustion focused on the Governing Vessel meridian experienced significant reduction of pain.
Moxibustion warms and invigorates yang energy and can help improve immune function. In the case of AS, this treatment protocol can help slow the progression of the disease, preventing inappropriate bone formation and reducing inflammatory responses.
A review of 26 studies that involved moxibustion treatment as an adjunct therapy for ankylosing spondylitis. The conclusion was that patients who had moxibustion in addition to conventional treatment fared better than those who did not receive moxibustion.
The British Acupuncture Council recommends TCM treatment for AS, as it has been shown to be effective at relieving back pain, without side effects.
One study of patients with ankylosing spondylitis who received acupuncture treatment and Chinese herb supplements, including herbal soak baths, found that people experienced pain relief and functional improvement.
A study that looked at 22 patients who received cupping therapy along with acupuncture and infrared heat lamps. The vast majority of the patients reported significant improvement in their pain symptoms.
Tuina therapeutic massage may also be helpful for helping to improve mobility and circulation.
A review of studies showed that acupuncture offers “unique advantages” in the treatment of ankylosing spondylitis, including localized pain relief, reduced inflammation, improvement of joint mobility, prevention of spinal deformity, and overall better quality of life.
Acupuncture Near Me for Ankylosing Spondylitis in West Los Angeles
Acupuncture can be an effective complementary treatment for many autoimmune disorders, including Sjogren’s disease, Lupus, as well as difficult-to-treat chronic pain conditions like fibromyalgia and complex regional pain syndrome (CRPS). Dr. Tan and Dr. Cai at Art of Wellness in West L.A. have over 35 years of experience helping patients find relief from all kinds of musculoskeletal pain.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.
How To Treat Baker’s Cyst With Acupuncture and TCM
By Qineng Tan, L.Ac., Ph.D. and Xiaomei Cai, L.Ac., Ph.D.

Swelling behind knee, lump behind knee, pain and swelling behind knee, knee stiffness? These can be Baker’s cyst symptoms. A Baker’s cyst in knee joint occurs when swelling in the knee forms a fluid-filled sac. Acupuncture treatment can help relieve Bakers cyst knee symptoms like knee pain and stiffness.
A Baker cyst, also known as a popliteal cyst, or synovial cyst, is a fluid-filled growth that develops in the back of the knee joint. In some cases, a Baker’s cyst causes knee pain, stiffness, and swelling; in other cases, there may be no Baker’s cyst signs and symptoms at all.
What causes Baker’s cyst? Usually, it is due to a knee injury, such as a cartilage tear, or arthritis in the knee joint. These types of problems cause inflammation in the knee, which can lead to the production of more synovial fluid than usual.
Synovial fluid is a thick, clear substance, similar to egg whites in consistency, that is present in the joints of the body to help lubricate their movements. It is produced by the synovium, a sort of bubble that surrounds joints like the knees, elbows, shoulders, and hips.
When the synovium becomes swollen and inflamed, due to injury or overuse of the joint, it may produce excess synovial fluid. In the case of a Baker’s cyst, the synovial fluid can build up in the knee joint, and form a bump, lump, or growth in the back of the knee.
People who have a history of knee injury, osteoarthritis, or rheumatoid arthritis may be more prone to developing Baker’s cysts.
Bakers cyst treatment is usually only indicated if a person is experiencing significant pain or limitation of movement. Acupuncture treatment can provide an adjunct or alternative Baker’s cyst therapy to help promote healing and relieve Baker’s knee symptoms.
Top 5 Baker’s Cyst Symptoms

Photo by Jenny Hill on Unsplash
Many people have a baker’s cyst knee without realizing it. If there is no pain, a person may not notice the lump behind knee.
Baker’s cyst signs and symptoms include:
- Knee pain, pain in the back of the knee
- Knee stiffness, stiff knee joint, especially when straightening the leg
- Swollen knee, swelling in knee joint
- Swelling goes away when knee is bent
- Pain and stiffness are worse after standing for a long time
More severe baker’s cyst symptoms could include redness and swelling, as the cyst gets larger.
In some cases, a baker’s cyst can rupture. If this happens, there may be swelling, redness, and a warm sensation in the calf area. Rupture of a baker’s cyst could cause pain or numbness in the calf, lack of blood flow to the lower leg, as the ruptured cyst could trap a nerve or artery in the knee or lower leg.
In extreme cases, a ruptured Baker’s cyst could lead to compartment syndrome, which could cause intense pain, foot drop, edema in the lower leg, and possibly, even an inability to move the foot or toes. If you believe your Baker’s cyst has ruptured, you should seek emergency care.
While, in most cases, a Baker’s cyst will eventually go on on its own, it is best to get a diagnosis and discuss your options. Acupuncture and TCM offer treatment of Baker’s cysts that is non-invasive and can help improve healing and prevent regrowth of the cyst.
Baker’s Cyst Treatment
Baker’s cyst signs and symptoms can be similar to those of a blood clot, or even a tumor. So, while a doctor can often diagnose a Baker’s cyst simply by palpating the area, they may also order imaging tests to be sure.
In many cases, doctors will prescribe over the counter pain medications and allow time for the cyst to go away on its own. You may be advised to limit activities that might aggravate the knee inflammation. Resting and elevating the knee for a few weeks might be recommended.
In some cases, a doctor may give cortisone injections to reduce knee swelling, or perform needle aspiration to drain the fluid from the cyst.
Surgery is generally only suggested in situations in which the knee pain has become chronic and inflammation does not seem to be going away.
Unfortunately, these medical treatments for Baker’s cyst may help bring relief, but it is quite common for the Baker’s cyst to come back again. Acupuncture treatment is not only a good way to bring symptomatic relief, but can help prevent the recurrence of Baker’s cysts.
Acupuncture has long been considered an excellent modality for treating knee pain due to all types of conditions. TCM offers an adjunct or alternative treatment for knee pain, without side effects that can come with pain medications or steroids.
Can Acupuncture Help Baker’s Cyst?

Acupuncture and TCM treatments with Chinese herb formulas have been used for centuries to treat knee injuries of all kinds.
According to TCM theory, arthritis in the knee that causes pain and stiffness is caused by stagnation that blocks the smooth flow of blood and Qi (life force energy). Acupuncture and herbs are used to address the underlying causes of blockages.
Injuries like a torn meniscus in the knee, or damage to the cartilage of the knee are very common, and it is also common for a person who has suffered such an injury to develop a Baker’s cyst later on. Full healing of cartilage can be helped with specific herbs that bring more nutrients to the damaged tissues.
Once a pattern of inflammation has begun, it can be difficult to get the swelling to go away. Small movements can trigger the inflammatory response if the area is not fully healed, and if other lifestyle habits are also causing a person to be prone to inflammation.
Chinese medicine looks at the situation holistically, treating the situation with acupuncture treatment, cupping, herbs, and nutrition, so that overall inflammation is reduced, and swelling and pressure is reduced, as well.
Herbal patches that are applied topically may be used in addition to herbal teas taken internally, to help relieve knee pain and swelling.
Cupping can also be helpful for healing and prevention of Baker’s cysts. One study compared patients with a popliteal cysts who were treated with acupuncture and cupping to patients who were given injections of prednisone. Both groups had high rates of effectiveness in terms of relief from the cysts, but recurrence of Baker’s cyst was significantly lower in the group that received TCM treatment as opposed to steroids.
Acupuncture Near Me for Baker’s Cyst, Los Angeles, CA
If you or someone you know has been suffering from knee pain and stiffness, due to a knee injury, arthritis, or diagnosed with Baker’s cysts on knee, it is worth seeking help from an acupuncturist experienced in working with orthopedic injuries, like Dr. Tan at Art of Wellness in West Los Angeles. TCM treatment for Baker’s cyst and other problems with the knee joint can not only help to relieve pain and increase range of movement; it can help prevent knee pain from coming back in the future.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.
How to Treat Cystic Fibrosis With TCM and Acupuncture
By Qineng Tan, L.Ac., Ph.D. & Xiaomei Cai, L.Ac., Ph.D.
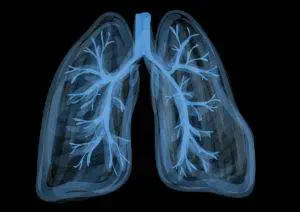
Cystic fibrosis (CF) is a genetic disease that causes phlegm or mucus in the body to be too thick and sticky, which can lead to malfunctioning of vital organs. Cystic fibrosis can cause infections and ultimately, damage to the lungs, heart, and digestive system. Acupuncture and TCM can provide complementary treatment for cystic fibrosis symptoms.
CF disease causes serious problems throughout a person’s system due to the production of abnormal mucus (sometimes spelled mucous). Mucous should be mostly made of water, so that it provides lubrication in and around the major organs. Mucus that does not have the right balance of water and salt can clog parts of the body, especially the airways, making it difficult to breathe. The thick mucus can also cause blockages in the digestive system.
Cystic fibrosis is caused by mutations of the CFTR gene, which provides the information for producing the CFTR protein. When this protein doesn’t work right, it can lead to the wrong amount of salt or water in the mucus. If mucus is too sticky, then organs like the lungs, intestines, and liver have a hard time doing their respective jobs. Thick mucus in the pancreas, in particular, can cause digestive problems, malnutrition, and can affect insulin production, leading to diabetes.
As recently as a few decades ago, it used to be that children with CF rarely lived into adulthood. Now, CF life expectancy has increased due to advances in cystic fibrosis treatment. Current cystic fibrosis life expectancy statistics show that the average person with CF will live into their mid-40s; there are now many senior citizens still living with CF, and there are more adults with cystic fibrosis than children.
There are many different types of cystic fibrosis treatment, which can help reduce symptoms and complications. Medical treatment for cystic fibrosis aims to change the quality of the mucus, clear mucus from the lungs, reduce chances of infection, and improve the absorption of nutrients from food. Acupuncture and other TCM treatment for cystic fibrosis can also be used to help improve these CF symptoms.
Cystic Fibrosis Symptoms
Signs of cystic fibrosis symptoms in infants may look different than CF symptoms in adults. A person is born with CF, but different symptoms may develop over time.

Symptoms of cystic fibrosis in children may include:
- Salty sweat, skin tastes salty
- Phlegmy cough, coughing up blood
- Wheezing, trouble breathing
- Poor growth, low weight, failure to thrive
- Greasy stool or constipation
- Gassy, stomach ache, pain in belly
- Finger clubbing, clubbed fingers, or clubbed toes
Other, deeper health problems may develop as children with cystic fibrosis grow, including: lung infections, sinus infections, pancreatitis, gallstones, liver disease, diabetes, rectal prolapse, or high blood pressure in the lung arteries that can lead to heart failure.
Most people are diagnosed with cystic fibrosis while they are still very young, but it is possible for a person to grow into adulthood without knowing they have CF.
Adults with cystic fibrosis may experience:
- Decreased immune function, low levels of antibodies
- Liver problems, cirrhosis
- Lack of digestive enzymes due to low functioning of the pancreas
- Intestinal blockages
- Low absorption of nutrients due to mucus in the intestinal tract
- Infertility in men; male infertility
- Bone disease, arthritis
Cystic Fibrosis Genetics
Cystic fibrosis is a chronic disease that is caused by a recessive gene. Cystic fibrosis inheritance means that both parents have a mutated copy of the CFTR gene; in other words, each parent is a cystic fibrosis carrier, even though in most cases, neither parent has CF or cystic fibrosis symptoms.
Cystic Fibrosis Diagnosis and CF Testing
Most newborn babies are tested for signs of cystic fibrosis in the U.S., so parents will usually learn that their child has CF soon after birth. This way, cystic fibrosis treatment can be implemented immediately, which offers the best chances of keeping CF disease under control.
Initial screening for CF involves first checking for high levels of IRT, a chemical protein released by the pancreas. High levels of IRT can be an indicator of CF or other problems with the pancreas; although, it can also be related to infant stress or premature delivery. If the IRT is high, then other tests will be performed.
A sweat test is considered the primary way to diagnose cystic fibrosis. Sweat is collected from the skin. If it shows high levels of salt, or chloride (a chemical component of salt), this is an indication that a person has CF.
Genetic testing, or CR carrier testing, will usually be performed in order to confirm the CF diagnosis, and so that the specific genetic defects that will affect the patient’s health are understood fully.
Cystic Fibrosis Treatment
Up until recently, most CF treatments were aimed at helping to provide symptomatic relief. Cystic fibrosis medications include drugs that can help thin mucus, bronchodilators to help open the airways, and antibiotics to help prevent and control infections. Many of these medications are inhaled through a nebulizer.
A cystic fibrosis vest is a machine worn around the chest that vibrates and can be used as a daily therapy to help clear mucus from the lungs.
More recent advances have led to the development of genetic therapies for cystic fibrosis. CFTR modulator therapies address the underlying CF causes having to do with cell membranes and the CFTR protein. This new treatment may be able to improve lung function in patients who have the most common form of CFTR gene mutation.
People with CF need to eat more calories and a higher fat diet in order to be able to maintain a healthy weight and get enough nutrients, so they are usually prescribed a special cystic fibrosis diet to help them achieve this.
Cystic fibrosis is a chronic illness that requires constant care. TCM and acupuncture can provide a meaningful adjunct treatment to medical therapies to improve quality of life and longevity.
Can Acupuncture Help Cystic Fibrosis?

Centuries before medical science began to understand how genetic diseases are passed down, TCM has acknowledged that certain conditions are part of a person’s constitution when they are born.
According to TCM theory, we are all born with Qi. Some Qi can be replenished (Postnatal Qi), and other Qi is given to us at birth in a finite amount (Yuan Qi, or Ancestral Qi).
Difficulty with breathing and digesting food causes people with CF to have a harder time replenishing Qi. They also have less of the finite type of Qi, so they must take extra care to preserve it. Because of this weaker Qi, the organ systems of the body have deficiencies that must be helped with nourishment and care. Kidney deficiency, which is related to the weaker Yuan Qi, can lead to lack of fluids in the body, as is typical in CF. TCM can help improve organ function through modalities like acupuncture, cupping, herbs, and nutrition.
TCM methods used in combination can help to clear phlegm from the lungs and other organs. This, in turn, will help a person fight off infections better.
Cupping, a modality that creates suction to increase circulation can help draw congestion from the lungs. Chinese herbs and the right nutrition program can help to improve the balance of fluids in the body, to help thin mucus.
Many adults with cystic fibrosis experience chest pain, gastrointestinal pain, and/or headaches. Acupuncture has been shown to decrease these types of pain.
Acupuncture Near Me for Cystic Fibrosis, Los Angeles Area
Living with a chronic illness is an everyday challenge. It is necessary for patients with Cystic fibrosis to build a team of healthcare professionals who can support them with the right treatment for their individual needs. An acupuncturist takes into consideration the whole person: their specific symptoms, and also their mental and emotional health. Regular visits with a TCM doctor can help alleviate the physical symptoms of CF, but also help maintain emotional balance, addressing feelings of depression and anxiety. If you or someone you know has cystic fibrosis, please consider adding acupuncture to your healthcare plan.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.