-
 Art of Wellness Acupuncture & Traditional Chinese Medicine (TCM)11704 Wilshire Blvd, Suite 295, Los Angeles, CA, 90025
Art of Wellness Acupuncture & Traditional Chinese Medicine (TCM)11704 Wilshire Blvd, Suite 295, Los Angeles, CA, 90025
myartofwellness@gmail.com310-451-5522 Office Hours
MonClosedTue7:30 am --4 pmWed7:30 am --4 pmThu7:30 am -- 4 pmFri7:30 am -- 4 pmSat7:30 am -- 4 pmSunClosedOur office opens from Tuesdays to Saturdays 7:30 am to 4 pm, will be closed on Memorial day, Independent day, Labor day, Thanksgiving day, Christmas and New year.
-
Recent Posts
- How to Treat De Quervain’s Tenosynovitis With Acupuncture and TCM
- Chinese New Year 2026: Year of the Horse
- Acupuncture and TCM Treatment for Perimenopause Symptoms
- How to Treat Insulin Resistance With Acupuncture and TCM
- How to Treat Metabolic Syndrome With Acupuncture and TCM
- How to Treat Syncope With Acupuncture and TCM
- How to Treat Thoracic Outlet Syndrome With Acupuncture and TCM
- How to Treat Dupuytren’s Contracture With Acupuncture and TCM
- How to Treat Nutcracker Syndrome With Acupuncture and TCM
- How to Treat Rosacea With Acupuncture and TCM
- How to Treat Perioral Dermatitis With Acupuncture and TCM
- Lymphatic Drainage With Acupuncture and TCM
- How to Treat Turf Toe With Acupuncture
- How to Treat Nerve Pain With Acupuncture and TCM
- How to Treat Watery Eyes With Acupuncture and TCM
- How to Treat Ovarian Cysts With Acupuncture and TCM
- Sign up to receive news and updates and get my free report:“The Top 10 Reasons to Try Acupuncture”

December 2025 M T W T F S S 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31
kidney
Acupuncture and TCM Treatment for Perimenopause Symptoms
By Xiaomei Cai, L.Ac., Ph.D. and Qineng Tan, L.Ac., Ph.D.

Changes in mood, sleep, energy levels, or menstrual cycle? Hot flashes, itchy skin, or joint pain? These can all be signs of perimenopause, the transitional period leading up to menopause. Acupuncture and Traditional Chinese Medicine (TCM) provide a holistic approach to managing perimenopause symptoms.
While everyone experiences the perimenopause transition differently, it is common to have disruptive perimenopausal symptoms that can affect your physical and emotional well-being. Acupuncture and herbs can help balance hormones, regulate the menstrual cycle, reduce stress, restore energy, and improve your quality of life.
What Is Perimenopause?
Perimenopause refers to the years leading up to menopause, when hormone levels, particularly estrogen and progesterone, begin to fluctuate. This transition often begins in a woman’s 40s, but can start earlier.
Perimenopause can last several years, with symptoms gradually intensifying until menstruation stops completely. “Menopause” is defined as having gone 12 months without a period, which means it technically is just one day! Most people with periods will experience perimenopause for years, and then be “post-menopausal” for up to a third of their lifetime.
Some doctors will recommend hormone replacement therapy (HRT) or medications to target specific symptoms. For some women, HRT is not recommended, due to their medical history. And some women prefer natural, non-pharmaceutical approaches.
Acupuncture and Chinese herbal medicine work by addressing the underlying imbalances that contribute to perimenopausal symptoms, offering a safe and effective alternative or adjunct treatment to hormone therapy.
Top 12 Most Common Perimenopause Symptoms

TCM practitioners look for diagnostic patterns based on the range of symptoms an individual is experiencing and then creates a treatment plan to balance the organ systems and correct the root problem that is causing them. With menopause and perimenopause, typical TCM diagnosis might be:
- liver and kidney yin deficiency
- kidney yang deficiency
- both yin and yang kidney deficiency
- disharmony of heart and kidney
- liver stagnation and spleen deficiency
- stagnation of liver qi
Insomnia
Trouble falling or staying asleep is one of the most common complaints in perimenopause. In TCM, sleep disruption often reflects Yin deficiency (lack of cooling, nourishing energy) or Heart–Kidney disharmony. Acupuncture helps calm the Shen (spirit) and regulate the nervous system, while herbal formulas and dietary guidance focus on nourishing Yin and calming the mind. Simple lifestyle suggestions—reducing late-day stimulants, winding down with gentle stretching or qigong, and keeping a cool, dark bedroom—are part of an integrated plan.
Anxiety
Perimenopausal anxiety often shows as persistent worry, tension, or a feeling of being “on edge.” From a TCM point of view this is frequently Liver Qi stagnation or Heart Shen disturbance. Acupuncture points to move Liver Qi and settle the heart, paired with calming herbs and breath-work, can substantially reduce anxiety and the physical tension that accompanies it.
Depression
Low mood or persistent sadness (depression) may be linked in TCM to Liver Qi stagnation, Spleen Qi weakness (fatigue and poor appetite), or Heart blood deficiency. Treatment is individualized: acupuncture to regulate the flow of Qi, herbal formulas to strengthen the Spleen and nourish the Heart, and lifestyle counseling—regular movement, sunlight, and social support—are all used to lift mood and restore resilience.
Itching / Pruritis
Itchy skin in perimenopause can be triggered by hormone-related dryness or underlying heat from Yin deficiency. TCM treats this by nourishing Yin, clearing deficient heat, and resolving any skin dampness. Topical herbal washes, internal formulas that nourish fluids, and acupuncture to balance the Skin and Lung channels are commonly used approaches.
Joint Pain (including hip and shoulder pain, frozen shoulder)
Joint aches and stiffness often flare during perimenopause, due to declining Yin and Lubrication for the tendons and joints. TCM diagnoses may include Wind-Cold-Damp invasion or Kidney/Liver deficiency affecting the sinews. Local and distal acupuncture, moxibustion when cold is involved, herbal anti-inflammatory formulas, and therapeutic tuina or gentle mobilization help reduce pain, improve circulation, and restore range of motion.
Hip Pain
In TCM, hip pain is frequently associated with Kidney deficiency (which governs the bones and joints) or Blood stasis. Treatments focus on nourishing Kidney essence and moving blood to relieve stiffness and referred pain. Clinical outcomes are often improved when acupuncture is combined with targeted exercises for hip stability.
Shoulder Pain / Frozen Shoulder
Frozen shoulder is treated as a painful obstruction (a kind of Bi syndrome) in TCM. Needling local shoulder points together with distal points that move Qi and break up stagnation can help restore mobility. Repeated, gentle treatment sessions with acupuncture, adjunct cupping or gua sha, and rehabilitative stretching often bring gradual, sustained improvement.
Acne
Hormone-driven acne in perimenopause can result from Liver Qi stagnation transforming into Heat or from Phlegm-Damp accumulation. TCM treatment clears Heat, transforms Phlegm, and supports digestion (the Spleen) so skin eruptions calm. Herbal formulas tailored to the pattern, dietary adjustments (reducing spicy/fried foods and dairy for some people), and acupuncture to regulate hormones are commonly used.
Brain Fog
Difficulty concentrating, forgetfulness, and mental fog often accompany hormonal transitions. In TCM this can be modeled as Qi and blood not adequately nourishing the brain (the “Sea of Marrow”), or as Kidney essence declining. Acupuncture to improve circulation and nourish Yin and blood, herbal support to improve mental clarity, and lifestyle strategies (sleep hygiene, structured routines, mild aerobic exercise) are used together to sharpen cognition.
Irregular Periods
Perimenopause often brings irregular cycles, heavier or lighter bleeding, and spotting. In TCM irregular menses result from Liver Qi stagnation, blood deficiency, or Yin-Yang imbalance. Treatment aims to regulate the menstrual cycle by harmonizing Liver and Spleen, nourishing blood, and, when needed, cooling excess heat. Acupuncture can help re-establish more predictable cycles over time while herbs address the underlying pattern.
Fatigue
Persistent low energy is commonly related to Spleen Qi deficiency in TCM (poor digestion and energy extraction) or to Kidney depletion. Acupuncture protocols focus on strengthening Spleen Qi and boosting overall vitality; herbs like astragalus-based formulas and dietary adjustments—regular, nourishing meals—support long-term recovery.
Hot Flashes and Night Sweats
Perhaps the most classic perimenopausal complaint, hot flashes reflect Yin deficiency with relative heat in TCM theory. Acupuncture has a strong evidence base for reducing the frequency and severity of hot flashes by modulating autonomic balance and calming the underlying deficient heat. Herbal formulas that nourish Yin and clear deficient heat, combined with dietary/lifestyle strategies (cooling foods, layered clothing, avoiding triggers), round out the approach.
Can Acupuncture Help Perimenopause?

Multiple clinical trials and systematic reviews support acupuncture’s effectiveness for common perimenopausal symptoms. For instance, a randomized controlled trial examining perimenopausal insomnia found that acupuncture significantly improved sleep quality, total sleep time, and reduced time to fall asleep compared to control groups. Another systematic review evaluating acupuncture for comorbid insomnia and depression reported moderate to strong benefits in sleep metrics and mood with low risk of adverse events.
In addition to the sleep and mood benefits, acupuncture has been studied for vasomotor symptoms (hot flashes). A meta-analysis pooling several trials showed that acupuncture reduced the frequency and severity of hot flashes more than sham acupuncture and often matched hormone therapy in effect size, with fewer side effects. These studies underscore acupuncture’s potential not only to alleviate surface symptoms but also to exert beneficial regulatory effects on hormonal and autonomic systems.
Perimenopause is a highly individual transition; two people can have the same complaint (like insomnia or hot flashes) for very different energetic reasons. That’s why TCM emphasizes tailored treatment—your acupuncture points, herbs, and lifestyle plan are selected based on your unique pattern. Acupuncture offers real physiologic benefits (calming the nervous system, improving sleep architecture, reducing inflammation) while herbs and diet support deeper rebuild of Yin, Blood, and Digestive Qi. Regular treatments over several months are often most effective, with maintenance “tune-ups” to keep symptoms at bay.
If you’re struggling with perimenopausal symptoms, acupuncture and TCM can be a safe, effective complement to conventional care. At Art of Wellness we create personalized plans that combine acupuncture, Chinese herbal therapy, nutritional guidance, and qigong to help you move through this transition more comfortably and regain balance.
Acupuncture Near Me for Perimenopause in West Los Angeles
If perimenopause is impacting your sleep, mood, skin, joints or day-to-day energy, please don’t hesitate to reach out. We’re happy to schedule a consultation to review your symptoms, discuss a personalized TCM treatment plan, and answer any questions about how acupuncture and herbal medicine can support you through this phase of life. Call or book online to get started.
At Art of Wellness Acupuncture in Santa Monica, we specialize in women’s health and menopause care. If you are experiencing symptoms of perimenopause, reach out today to schedule a consultation. Together, we can create a personalized treatment plan to help you feel more like yourself again.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.
Can Acupuncture Help Bad Breath?
By Qineng Tan, L.Ac., Ph.D. and Xiaomei Cai, L.Ac., Ph.D.

Dry mouth, coated tongue? Bad taste in your mouth, breath is always bad? There may be a deeper reason behind halitosis. Acupuncture and TCM can help correct the internal imbalances that are the root cause of bad breath.
How To Get Rid of Bad Breath
Looking for how to get rid of bad breath? Conventional medicine often sees bad breath as a dental issue, related to oral hygiene, gum disease, and bacteria on your tongue and in your mouth.
Recommendations for treating bad breath typically include using antibacterial mouth rinses and toothpastes, scraping your tongue, and flossing.
But what causes bad breath and dry mouth?
Bad Breath Causes

There are many health conditions that can cause bad breath, including:
- GERD – with acid reflux, some of the contents of the stomach come back up into the esophagus, which can smell strong.
- Diabetes – contributes to gum disease and bacterial growth in the mouth because of high glucose levels and poor blood flow to gums.
- Liver disease – breath may have a sulfurous, rotten egg smell, because toxins are not being adequately filtered by the liver.
- Kidney disease – can cause a metallic taste in the mouth, because minerals are not being filtered out through the kidneys.
- Sjogren’s Syndrome – parotid gland dysfunction leads to dry mouth.
- Sinusitis – mucus from sinus infection can smell bad as it drips into the back of the throat.
- Tonsillitis or tonsil stones – infected pus around the membranes of the tonsils can smell.
Other symptoms that often accompany bad breath include:
- Burning sensation on the tongue
- Need to clear your throat all the time
- Buildup on teeth, coated tongue
- Thick saliva
- Bad taste in mouth: metallic taste, sour taste, or bitter taste
Addressing these health issues can help clear up halitosis. But, what if you are experiencing frequent bad breath, and none of these health problems are the cause?
Underlying Causes of Bad Breath

According to TCM theory, bad breath usually arises from imbalances in the internal organ systems. Acupuncture treatment and herbal remedies can address the root causes of bad breath, so that it doesn’t come back.
In TCM, we consider “heat,” “wind,” “dampness,” “dryness,” and so on to be pathogenic factors that can either get into the body from external causes, or arise within the organ systems due to imbalances in Yin and Yang energies, or the obstruction or stagnation of Qi (life force energy).
Dryness and heat are the primary pathogenic factors that might lead to bad breath becoming a problem.
These words sound metaphorical, but they describe the nature of how problems occur within the human body and produce various symptoms. “Fire” or “heat” produces redness, swelling, eruptions of red bumps, thirst, excessive acid, etc.
When we say that pathogenic factors can arise from within, we are also acknowledging that emotions affect our physical and mental health, and vice versa.
Liver fire, or excess Yang energy in the Liver, for example, can arise due to dietary habits, like too much spicy food, or changes in weather, like warming temperatures in the springtime.
Liver heat is also related to feelings of anger and frustration. So, a lot of emotional stress and repressed anger can lead to liver fire problems.
Hot weather can contribute to feeling irritable. We must look at all sides of the problem in order to treat Liver fire and reduce uncomfortable symptoms, like trouble sleeping, and dry mouth.
Patterns of disharmony that can lead to bad breath as a symptoms include:
- Dry Intestine – leads to constipation and dry stool, dry throat and mouth, dizziness, hemorrhoids
- Stomach heat – thirsty all the time, craving for cold drinks, hungry all the time, canker sores, stomach pain, acid reflux, vomiting, feeling hot, acne breakouts
- Excess phlegm – tightness in chest, brain fog, dizziness
Sometimes one imbalance can lead to another. For example, liver fire can lead to fire in the lungs, causing chest pains and respiratory problems. Liver fire moving into the heart can cause angry outbursts, dry throat, and a bitter taste in your mouth.
TCM Nutrition to Address Bad Breath
Rather than simply telling you not to eat garlic, your acupuncturist will talk with you about eating the right foods to cool down the specific type of heat that is affecting your health. In TCM, we view certain foods as being “warming” or “cooling.” Eating more cool and neutral foods and avoiding heat-producing foods can help with halitosis.
An acupuncture practitioner will also assemble an herbal formula designed to address the organ system imbalances that seem to be causing problems.
Acupuncture Near Me for Bad Breath in West Los Angeles
Having bad breath can impede your social life and even your career. Experiencing dry mouth on a regular basis is very uncomfortable. It is important to address these issues, as they are likely an indication that there is something happening deeper under the surface. Please do not hesitate to reach out to us at Art of Wellness Acupuncture in Los Angeles, so that we can resolve this issue and help you feel better and more confident in your day to day life.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.
How to Treat Splenomegaly (Enlarged Spleen) With Acupuncture and TCM
By Qineng Tan, L.Ac., Ph.D. and Xiaomei Cai, L.Ac., Ph.D.
Left side abdominal pain that is tender to the touch? Feeling full after eating a small amount? Signs of anemia, bleeding easily? These may be enlarged spleen symptoms. Acupuncture and TCM can help with splenomegaly, along with spleen function and swollen spleen symptoms.
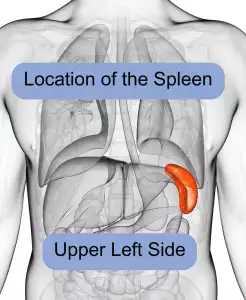
Splenomegaly is the medical term for an enlarged spleen. In conventional medical wisdom, the spleen is an organ that stores and filters blood, regulating the amounts of red blood cells, white blood cells, and platelets that are in circulation.
The spleen removes waste products and damaged blood cells from the bloodstream. It also produces antibodies (white blood cells) that fight germs and infection.
The spleen is located inside the left side of the ribcage, just above the stomach. Usually, the spleen is about the size of your fist—on average, about 12 centimeters long.
People often will not be aware of an enlarged spleen, but in some cases, there will be noticeable signs, such as pain in upper left abdomen and feeling “full.”
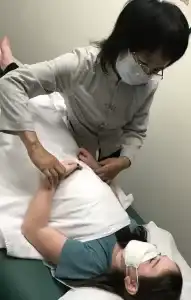
Spleen function is considered very important for overall health and happiness in TCM. Acupuncture treatment and Chinese herbs can provide an adjunct or alternative treatment for enlarged spleen.
Enlarged Spleen Symptoms
The most common swollen spleen symptoms include:
- Left upper quadrant pain, pain behind left ribs, left abdominal pain (upper abdomen), left side abdominal pain
- Pain that radiates to the left shoulder
- Feeling full even when you haven’t eaten
- Feeling full after eating only a small amount
- Anemia, low red blood cell count
- Bruise easily
- Bleeding easily
- Fatigue
- Catch colds frequently or suffer from other infections often
If you experience tenderness or serious left abdominal pain and feel dizzy, and/or have a rapid heartbeat, it is important to seek care immediately. These could be signs of ruptured spleen, which can lead to internal bleeding that could be life-threatening.
Enlarged Spleen Causes

There are several different conditions that can cause the spleen to become enlarged. What causes a big spleen, or should we say, bigger spleen?
Some of the health issues that can cause splenomegaly include:
- Liver cirrhosis, or other liver disease
- Viral hepatitis, Mononucleosis, or other viral infections
- Different types of hemolytic anemia
- Blood cancers, including: polycythemia vera and other myeloproliferative neoplasms, Leukemia, lymphoma, Hodgkin’s disease
- Blood clot near the spleen or liver
- Autoimmune disorders, including Lupus or Sarcoidosis, or rheumatoid arthritis (RA)
- Malaria, or other parasitic infections
- Bacterial infections
- Gaucher disease or Niemann-Pick disease
Medical Treatment for Enlarged Spleen
The treatment of splenomegaly in Western medicine primarily depends on addressing the underlying cause of the condition.
When an enlarged spleen is caused by infections like viral hepatitis or mononucleosis, the focus is typically on treating the infection itself. Antiviral medications may be prescribed to manage viral hepatitis, while mononucleosis, caused by the Epstein-Barr virus, usually requires supportive care. Rest, hydration, and over-the-counter pain relievers like acetaminophen or ibuprofen may be recommended to alleviate symptoms. In some cases, particularly when there’s a risk of the spleen rupturing, patients may be advised to avoid contact sports or strenuous activities.
For blood disorders that cause an enlarged spleen, treatment typically involves managing the specific blood condition. For example, in hemolytic anemia, where red blood cells are destroyed faster than they can be produced, treatments may include blood transfusions, corticosteroids to suppress the immune system, or medications like rituximab.
In conditions like polycythemia vera, where there’s an overproduction of red blood cells, treatment might involve phlebotomy (removing blood from the body) to reduce blood volume, or medications like hydroxyurea to suppress the bone marrow’s production of blood cells.
When liver disease such as cirrhosis is the cause of splenomegaly, the treatment approach focuses on managing the liver condition. Cirrhosis management may include lifestyle modifications such as reducing alcohol intake, using medications to control liver damage, and managing complications like portal hypertension. In severe cases, a liver transplant may be considered. Controlling the liver condition can help reduce spleen enlargement.
In cases where the spleen enlargement is due to cancers like leukemia or lymphoma, treatment usually involves chemotherapy, radiation therapy, or targeted drug therapies to address the cancer. The goal is to reduce the size of the spleen by shrinking the cancerous cells that are contributing to its enlargement. In certain situations where the spleen is significantly enlarged and causing symptoms, or if it’s not responding to other treatments, splenectomy (surgical removal of the spleen) might be recommended.
Autoimmune disorders like lupus or rheumatoid arthritis can also cause splenomegaly. Treatment for these conditions often involves immunosuppressive medications such as corticosteroids, methotrexate, or biologic agents that target specific parts of the immune system. By controlling the underlying autoimmune disorder, the symptoms associated with spleen enlargement can often be managed effectively.
When does an enlarged spleen need to be removed?
In some cases, if the spleen is severely enlarged or if it’s causing significant symptoms or complications (such as a high risk of rupture), a splenectomy may be considered. This surgical procedure involves removing the spleen entirely. While splenectomy can relieve symptoms and prevent complications, it also has long-term implications, as the spleen plays an important role in the immune system. Patients who undergo splenectomy may require vaccinations and prophylactic antibiotics to reduce the risk of infections.
Unless the spleen is ruptured, in most cases, a splenectomy is not necessary. Trying a holistic approach with TCM and acupuncture may be able to help relieve symptoms and improve spleen function.
Can Acupuncture Help Enlarged Spleen?

Traditional Chinese Medicine takes a different few of key organs and organ systems than we are used to in modern medicine.
In TCM, the spleen is considered vital to the digestion of food, working in harmony with the stomach. The spleen is also partially responsible for the transport of blood and water throughout the body, delivering nutrition to the muscles.
The spleen is also vital to the proper excretion of waste. When there is a buildup of excessive fluids or “dampness” in the body, it is often due to a deficiency of the spleen.
Fatigue and a sense of fullness after eating are considered signs of spleen deficiency, which can affect whether or not other organs are getting the nutrition they need.
Problems with the spleen may also be related to the liver and/or the stomach, so the acupuncture practitioner will carefully look at all of a patient’s presenting symptoms to determine the appropriate diagnostic pattern and course of treatment.
In TCM, organs are related to certain emotions, and the spleen is connected to anxiety. Thus, worrying, overthinking, and other manifestations of anxiety are believed to negatively impact the spleen.
TCM treatment to help strengthen spleen function may focus on clearing stagnation and dampness, and improving circulation of blood and Qi. Your acupuncture provider can develop a course of treatment with acupuncture and herbs to address the underlying causes of an enlarged spleen, while also helping to relieve any symptoms of splenomegaly.
Acupuncture for Enlarged Spleen Near Me in West Los Angeles
If you are experiencing enlarged spleen symptoms, acupuncture and TCM offer holistic approaches that can support spleen function and address the root causes of various health issues. At Art of Wellness, our experienced practitioners can help tailor a treatment plan to your unique needs. Contact us today to learn more about how TCM can benefit your health and well-being.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.
How to Treat Bone Spurs With Acupuncture and TCM
By Qineng Tan, L.Ac., Ph.D. and Xiaomei Cai, L.Ac., Ph.D.

Heel pain when walking? Numbness in arms or legs? Hip pain? These can all be signs of bone spurs, or osteophytes—bony projections that develop around joints or along the spine. Acupuncture and TCM can help alleviate pain and tingling related to heel spurs and bone spurs on spine,and help to prevent further growth of bone spurs.
Bone spurs are essentially extra bone tissue that grows around the edges of bones. This happens most commonly where two different bones meet in a joint. Bone spurs can grow in many areas: knees, hips, bone spurs on feet, shoulder, ankle, or bone spur in back.
What Is the Root Cause of Bone Spurs?
Osteoarthritis is a degenerative condition that causes cartilage to wear down over time. Sometimes bone spurs develop as the body’s way of making up for loss of cartilage in a particular area, trying to fill in the gap.
Bone spurs can also grow due to pressure on a bone, which can either be due to repetitive stress from movement (sports, dancing, etc.), extra weight because of obesity, or wearing shoes that rub or pinch the heel or top of the foot.
Maybe you’ve noticed foot spurs on heel. Heel spurs often relate to plantar fasciitis—inflammation in the ligaments of the foot that causes heel pain. Bone spur heel can develop as the body’s reaction to plantar fasciitis, causing sharp pain in the foot.
You might feel a lump or bump growing on the top of your foot or on one of your toes. Bone spurs in foot or heel are very common, especially as people age. The older you are, the higher your risk of developing bone spurs.
Having flat feet can also increase the risk of bones spurs on feet, as this condition puts extra stress on the many small bones and joints in your feet.
Osteophytosis of the spine can develop in the neck (cervical spine), mid-back (thoracic spine), or lower back (lumbar spine), potentially causing pain, stiffness, and nerve compression, leading to tingling or numbness in the arms and/or legs.
Bone Spur Symptoms

Many people have bone spurs without realizing it, because bone spurs don’t necessarily cause pain. In other cases, bone spurs can cause serious, debilitating pain, making it difficult to walk.
The most common signs of bone spurs include:
- Stiffness
- Redness and swelling around the bone spur
- Stiff joints
- Weakness in limbs
- Tingling or numbness in limbs
- Corns on the toes
- Difficulty standing or walking
Heel Spur Treatment
Bone spurs are typically diagnosed through physical examination and imaging studies, such as X-rays, MRI, or CT scans. These tests help determine the size and location of the bone spur and assess the extent of any associated damage to surrounding tissues, such as cartilage, muscles, or nerves.
Medications like ibuprofen or naproxen are commonly prescribed to reduce pain and inflammation. Corticosteroid injections may also be used to provide temporary relief from pain.
In severe cases, surgical intervention may be recommended. Procedures such as a bone spur removal (osteophyte excision) or joint replacement (in cases of severe osteoarthritis) may be performed. In some cases of heel spurs, this is combined with plantar fascia release surgery.
Most bone spurs, however, do not require surgery. It is possible to relieve pain and pressure caused by bone spurs and prevent them from growing bigger. Acupuncture and TCM can help by addressing the root cause of bone spurs.
Can Acupuncture Help Bone Spurs?

In Traditional Chinese Medicine (TCM), bone spurs are viewed as the result of imbalances within the body, particularly related to deficiencies in the Kidney and Liver organ systems.
What deficiency causes bone spurs?
According to TCM theory, the Kidneys govern the bones and produce marrow, which nourishes the bones. This concept of the “kidney” is very different from the way we think of it in modern medicine; it is more of a functional concept of how water is metabolized in the body, and how it relates to growth, development, and aging. Kidney deficiency can lead to weakened bones and the development of osteophytes.
Herbs that nourish the kidney system will be combined with acupuncture treatment. Specific acupoints can be used to stimulate the parathyroid gland, which plays a role in calcium utilization.
Acupuncture treatment can help provide pain relief for many orthopedic conditions that cause joint pain or bone pain, including tennis elbow, bursitis/hip pain, and arthritis.
One case study of a woman suffering from heel pain that had not resolved with conventional treatments of local steroid injections. After receiving regular acupuncture treatments over a course of six months, the patient reported that her pain had gone from an 8 on the pain scale to a 3. Radiology imaging showed, after the course of acupuncture treatment, that the bone spur was no longer in evidence.
Your TCM practitioner may recommend eating a diet that supports bone health, including foods that are rich in calcium, magnesium, and other essential nutrients. Foods that nourish the Kidneys, such as black beans, walnuts, and seaweed, will usually be emphasized.
Acupuncture Near Me for Bone Spurs in Los Angeles
Acupuncture and Traditional Chinese Medicine provide a holistic and effective way to manage and treat bone spurs. Drs. Tan and Cai at Art of Wellness in West L.A. have over 35 years of experience helping people find relief from bone pain due to all kinds of conditions. Whether you’re dealing with heel spurs, spinal osteophytes, or foot spurs, TCM can be an integral part of your treatment plan, offering a natural and holistic approach to long-term bone health.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.
How To Treat Pelvic Pain With Acupuncture and TCM
By Xiaomei Cai, L.Ac., Ph.D. and Qineng Tan, L.Ac., Ph.D.

Abdominal pain or groin pain? Painful urination or menstrual pain? Bloated stomach? Pain during sex or pain after sex? These can be signs of an inflamed pelvis, or chronic pelvic pain syndrome (CPP or CPPS). Acupuncture and TCM offer a way to treat many different causes of pelvic pain.
Pelvic pain is often related to problems with the reproductive organs (uterus or ovaries). Sometimes it can be due to a pelvic infection, pelvic congestion syndrome, or pelvic inflammatory disease. In other cases, chronic pelvic pain can be caused by problems with the digestive tract or urinary system.
Determining the cause of pelvic pain and finding an effective treatment can sometimes be challenging. TCM and acupuncture offer a holistic approach to treating pelvic pain.
Top 10 Causes of Pelvic Pain
Pelvic pain can arise from a multitude of conditions, each presenting its own set of symptoms.
Common causes of occasional or intermittent pelvic pain are menstrual cramps and ovulation pain (mittelschmerz).
Various types of pelvic pain are associated with pregnancy, as well, particularly hip pain, groin pain and pressure, bladder pressure, and uterus pain.
A gallbladder attack can cause severe pelvic pain.
These are some of the most common causes of chronic pelvic pain in women or AFAB:
- Endometriosis: This condition occurs when tissue similar to the lining of the uterus grows outside of the uterus, causing severe menstrual pain, pelvic pain, pain during intercourse, and fertility issues.
- Ovarian Cysts: These fluid-filled sacs can develop on the ovaries, often leading to bloating, pelvic pain, and discomfort during bowel movements.
- Kidney Stones: Hard mineral deposits in the kidneys can cause excruciating pain in the lower abdomen and groin, painful urination, and blood in the urine.
- Uterine Fibroids: These non-cancerous growths in the uterus can cause heavy menstrual bleeding, pelvic pressure or pain, and frequent urination.
- Pelvic Inflammatory Disease (PID): An infection of the female reproductive organs that causes lower abdominal pain, fever, unusual discharge, and pain during intercourse or urination.
- Urinary Tract Infection (UTI): Infections in the urinary system can cause pelvic pain, a burning sensation during urination, frequent urination, and cloudy urine.
- Interstitial Cystitis (IC): A chronic bladder condition causing bladder pressure, pelvic pain, and a frequent need to urinate.
- Diverticulitis: Inflammation or infection of small pouches that can form in the intestines, leading to severe abdominal pain, fever, and digestive issues.
- Colitis: Inflammation of the colon, often causing abdominal pain, diarrhea, and bloating.
- Irritable Bowel Syndrome (IBS): A gastrointestinal disorder that leads to cramping, abdominal pain, bloating, gas, and diarrhea or constipation.
Sometimes pelvic pain can be caused by muscles or ligaments, such as tightness or spasms in the pelvic floor.
Pelvic adhesions, scar tissue, or fascia in the pelvic region can cause pelvic pain and inflammation.
Generalized pain disorders like fibromyalgia or ME/CFS, can flare up in the pelvic area.
For some people, PTSD and other mental health conditions can trigger pelvic pain.
Typically, medical treatment for pelvic pain involves the use of NSAIDs, or pain medication, to help relieve symptoms. Sometimes doctors will prescribe antidepressant medications or opioids to deal with persistent pelvic pain.
In some cases, physical therapy, such as pelvic floor therapy, may be recommended.
TCM and acupuncture offer an effective alternative treatment for pelvic pain.
Can Acupuncture and TCM Help Pelvic Pain?
It can be difficult to find relief from pelvic pain. Many conditions that cause pain in the pelvis and reproductive organs are often overlooked by medical practitioners. For example, many women and AFAB suffer for years before finally getting a diagnosis for endometriosis.
Pelvic Pain in Women and AFAB
In Traditional Chinese Medicine (TCM), pelvic pain conditions like endometriosis are viewed as imbalances within the body’s organ systems, particularly the liver and kidney.
Dysmenorrhea, or painful menstruation, is often linked to Qi and blood stagnation, potentially caused by pathogenic factors such as cold and dampness, as well as emotional stress leading to liver stagnation. Acupuncture and herbal treatments aim to restore balance by promoting the flow of Qi and blood, influencing hormone production naturally.
Studies have shown that acupuncture can significantly reduce menstrual pain and regulate cycles, with high success rates and low recurrence when used consistently over time. Herbal remedies further support this process by providing essential nutrients and reducing inflammation.
Acupuncture and TCM have proven effective in treating various pelvic pain conditions, including uterine fibroids and PCOS. Clinical research demonstrates that acupuncture reduces prostaglandin levels, alleviating cramps and regulating the menstrual cycle. Techniques such as electroacupuncture and auricular acupuncture have shown high efficacy in managing dysmenorrhea (painful periods).
Urinary Pain Relief with TCM
In Traditional Chinese Medicine (TCM), the bladder’s function is closely connected to the kidney and spleen, which supply yang energy to warm and support the bladder. Deficiency in Kidney Qi, often due to prolonged illness or repeated untreated urinary tract infections (UTIs), can weaken the bladder, making it unable to hold urine effectively. This can also lead to bladder contraction and increased sensitivity.
Painful urination may arise from physical trauma, such as difficult childbirth, which impacts both physical and emotional health. Additionally, emotional distress can cause stagnation of Liver Qi, particularly if it leads to excess heat, further disrupting bladder and pelvic floor functions.
When treating interstitial cystitis (IC), an acupuncturist assesses a range of symptoms to determine the underlying causes of bladder pain. For example, fatigue, tinnitus, and cold extremities indicate Kidney Yang deficiency, while symptoms like constant thirst, allergies, warm hands, and anxiety suggest excess Kidney Yang heat.
Treatment protocols typically include acupuncture to alleviate bladder pain and balance organ system functions, supplemented by techniques like moxibustion and electro-acupuncture. Studies have shown that regular acupuncture sessions can significantly reduce urinary frequency and alleviate pelvic pain symptoms.
Pelvic Pain Colitis
In TCM, colitis and ulcerative colitis are viewed as conditions caused by imbalances that lead to heat, dampness, or blood stasis in the large intestine. TCM treatments focus on using acupuncture and herbs to reduce inflammation, clear heat, and eliminate dampness. Acupuncture points are selected to relieve symptoms like pain, bloating, and diarrhea.
For diverticulitis, TCM emphasizes diagnosing the root causes of symptoms such as abdominal pain, nausea, constipation, and diarrhea. According to TCM theory, these symptoms can be linked to stagnant Qi or blood and pathogenic forces like dampness, heat, or cold. Treatment often involves strengthening the spleen to improve nutrient absorption and energy conversion, which is crucial for resolving diarrhea and other digestive issues. Acupuncture and moxibustion are used to relieve symptoms, reduce inflammation, and boost immune function. Dietary changes, guided by TCM principles, are also essential to address excess heat or dampness in the gastrointestinal system and maintain overall health.
Pelvic Pain Kidney Stone

In TCM, kidney stones fall under the category of “Shilin” conditions, characterized by difficult urination. Herbal medicines are used to balance electrolyte minerals, which helps prevent stone formation in the urinary tract.
Acupuncture provides an anesthetic effect, helping to relieve the intense pain associated with kidney stones while other treatments work to reduce and prevent new stone formation. Acupuncture and acupressure can alleviate severe pelvic pain caused by various urinary and reproductive system conditions, as well as reduce anxiety and depression associated with severe pain.
Not only is acupuncture an effective modality for treating pain conditions, but many people find emotional relief, too, when a practitioner is willing to listen carefully and validate their experience. Drs. Cai and Tan at Art of Wellness have over 35 years of experience helping patients with all types of pain. Their caring and attentive bedside manner goes a long way towards helping patients feel more comfortable and confident in their own ability to heal.
Acupuncture for Pelvic Pain Near Me in West Los Angeles
At Art of Wellness near Santa Monica, Dr. Cai has unique expertise in treating women’s health issues of all kinds, including menstrual pain, female infertility, PCOS, and endometriosis. With acupuncture, herbal medicine, and nutrition, our acupuncture practitioners are able to help people find relief from pelvic pain of all kinds.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.