-
 Art of Wellness Acupuncture & Traditional Chinese Medicine (TCM)11704 Wilshire Blvd, Suite 295, Los Angeles, CA, 90025
Art of Wellness Acupuncture & Traditional Chinese Medicine (TCM)11704 Wilshire Blvd, Suite 295, Los Angeles, CA, 90025
myartofwellness@gmail.com310-451-5522 Office Hours
MonClosedTue7:30 am --4 pmWed7:30 am --4 pmThu7:30 am -- 4 pmFri7:30 am -- 4 pmSat7:30 am -- 4 pmSunClosedOur office opens from Tuesdays to Saturdays 7:30 am to 4 pm, will be closed on Memorial day, Independent day, Labor day, Thanksgiving day, Christmas and New year.
-
Recent Posts
- How to Treat De Quervain’s Tenosynovitis With Acupuncture and TCM
- Chinese New Year 2026: Year of the Horse
- Acupuncture and TCM Treatment for Perimenopause Symptoms
- How to Treat Insulin Resistance With Acupuncture and TCM
- How to Treat Metabolic Syndrome With Acupuncture and TCM
- How to Treat Syncope With Acupuncture and TCM
- How to Treat Thoracic Outlet Syndrome With Acupuncture and TCM
- How to Treat Dupuytren’s Contracture With Acupuncture and TCM
- How to Treat Nutcracker Syndrome With Acupuncture and TCM
- How to Treat Rosacea With Acupuncture and TCM
- How to Treat Perioral Dermatitis With Acupuncture and TCM
- Lymphatic Drainage With Acupuncture and TCM
- How to Treat Turf Toe With Acupuncture
- How to Treat Nerve Pain With Acupuncture and TCM
- How to Treat Watery Eyes With Acupuncture and TCM
- How to Treat Ovarian Cysts With Acupuncture and TCM
- Sign up to receive news and updates and get my free report:“The Top 10 Reasons to Try Acupuncture”

December 2025 M T W T F S S 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31
Inflammation
How to Treat De Quervain’s Tenosynovitis With Acupuncture and TCM
By Qineng Tan, L.Ac., Ph.D. and Xiaomei Cai, L.Ac., Ph.D.
Sore thumb? Swelling around the thumb? Wrist pain on thumb side? These could all be symptoms of De Quervain’s Tenosynovitis, or inflammation in the thumb tendons. Acupuncture and TCM provide natural alternative De Quervain’s tenosynovitis treatment, to help relieve pain and improve mobility.
What Is Tenosynovitis?
Tendons are strong, flexible tissues that connect muscles to bones. Tendons are protected by sheaths, or synovial membranes. When the sheaths become inflamed, they can swell and become less able to stretch and move freely.
Wrist pain, hand pain, ankle pain, and foot pain can all be caused, in some situations, by tenosynovitis, because these are parts of the body where the tendons are long and do a lot of work. There are synovial sheaths protecting tendons all over your body, though, and anytime they become inflamed, this can be referred to as “tenosynovitis.”
What causes De Quervain’s tenosynovitis? The causes of tenosynovitis are not always apparent. Inflammation can occur due to overuse of the joints, or repetitive motion, or an injury or strain. Infections and other health problems that contribute to overall inflammation can also cause De Quervain’s disease to develop (such as rheumatoid arthritis or diabetes).
Tenosynovitis can also be related to hormonal fluctuations and imbalances, particularly in women. This condition is sometimes referred to as “mother’s wrist,” because it is more common in postpartum women, and also during the perimenopause transition.
De Quervain refers specifically to inflammation of the sheaths that protect the tendons of the thumb, and can lead to pain and swelling around the base of the thumb and the wrist.
Conventional Medical Treatment for De Quervain’s Tenosynovitis
In most cases, conventional treatment for De Quervain’s tenosynovitis focuses on reducing inflammation in the tendon sheath and preventing further irritation. Doctors typically begin with conservative approaches such as rest, activity modification, and immobilizing the thumb and wrist with a splint or brace. By limiting the motion of the inflamed tendons, the sheath has a chance to calm down and heal.
NSAIDs, such as ibuprofen or naproxen, may be recommended to help reduce swelling and ease pain. For more persistent symptoms, corticosteroid injections are often used to decrease inflammation quickly. In many cases, these injections can provide temporary relief, but symptoms sometimes return, especially if repetitive motions continue.
In severe or longstanding cases that do not respond to conservative care, surgery may be suggested. A De Quervain’s release procedure involves opening the tendon sheath to relieve pressure on the tendons and restore normal gliding. While generally effective, surgery carries risks such as scarring, nerve irritation, or reduced grip strength.
Although these treatments can provide relief, you might want to seek alternatives that address both the inflammation and the underlying imbalances contributing to chronic tendon irritation. Acupuncture and Traditional Chinese Medicine can help relieve the pain of De Quervain’s tenosynovitis, while also addressing the underlying causes of inflammation.
How Hormones Affect De Quervain’s Tenosynovitis

Interestingly, De Quervain’s is more common in women, especially during pregnancy, postpartum, and perimenopause. Hormonal fluctuations—particularly changes in estrogen levels—appear to influence tendon and connective tissue health. Studies have shown that estrogen receptor beta (ERβ) is expressed in tendon tissues, and changes in estrogen levels may alter tendon metabolism, collagen turnover, and inflammatory signaling. Lower estrogen levels, or rapid fluctuations such as those occurring postpartum or during perimenopause, may make tendons more susceptible to swelling and irritation.
This explains why many new mothers develop De Quervain’s (“mother’s wrist”). Repetitive lifting of a child, combined with hormonal changes, can create the environment for tendon sheath inflammation. Acupuncture and TCM can be especially helpful for these patients because treatment addresses both local inflammation and the systemic hormonal imbalances that contribute to tendon vulnerability.
Acupuncture and TCM Treatment for De Quervain’s
In Traditional Chinese Medicine, De Quervain’s tenosynovitis is often associated with Qi and Blood stagnation in the wrist and thumb. When the flow of Qi is blocked, whether from overuse, strain, repetitive movements, or an underlying deficiency, the tendons are not receiving adequate nourishment. This lack of nourishment leads to stiffness, swelling, and pain along the meridians.
The affected area overlaps primarily with the Lung meridian (which runs along the thumb) and the Large Intestine meridian (which crosses the wrist). If these channels become obstructed, pain and restricted motion occur.

In some patients, underlying Liver Blood deficiency or Kidney deficiency can weaken the tendons, making them more prone to inflammation. Others may present with Dampness or Heat accumulation, leading to swelling, burning pain, and difficulty gripping.
TCM treatment not only targets the painful wrist but also restores balance throughout the body, helping to prevent recurrence.
How Acupuncture Helps De Quervain’s Tenosynovitis
Acupuncture is widely used for hand and wrist pain, and research supports its effectiveness for tendon inflammation. Clinical studies have shown that acupuncture helps reduce pain, improve grip strength, and restore normal tendon movement by increasing microcirculation around the sheath, reducing local inflammation, and promoting healing of soft tissues.
One controlled study found that acupuncture significantly reduced wrist pain and improved functional mobility in patients with De Quervain’s, performing as well as or better than splinting alone.
Other research demonstrates that acupuncture modulates inflammatory pathways, including cytokines and neuropeptides involved in tendon irritation (as reviewed in the study from Frontiers in Pharmacology).
Electroacupuncture may be especially helpful for stubborn cases by stimulating deeper tissues. Patients often experience noticeable improvement in pain and mobility within a few sessions.
Moxibustion may be used to warm the channels and promote better circulation, especially for chronic cases with Cold-Damp stagnation. Cupping around the forearm and upper arm can help release tension in the muscles that control thumb movement. Tui Na massage techniques help reduce adhesions around the tendon sheath and improve range of motion.
These manual therapies complement acupuncture by addressing muscle imbalances and promoting the smooth movement of tendons along the radial side of the wrist.
Chinese herbal formulas may be prescribed to address inflammation and support tendon repair.
Topical herbal liniments or plasters can also be applied directly to the wrist to promote circulation and relieve pain.
Acupuncture treatment is highly individualized. Some patients require more focus on inflammation reduction, while others need systemic support for hormonal balance, postpartum recovery, or chronic overuse patterns. By addressing both tendon inflammation and whole-body imbalances, acupuncture offers a comprehensive approach that can improve healing and prevent future flare-ups.
Acupuncture for De Quervain’s Tenosynovitis Near Me in West Los Angeles
If thumb and wrist pain are limiting your daily activities, acupuncture and Traditional Chinese Medicine can offer natural, effective relief. Whether your symptoms began after repetitive work, new parenthood, or hormonal changes, TCM provides a personalized, holistic plan to reduce inflammation and restore comfortable movement.
Contact Art of Wellness, near Santa Monica, to schedule a consultation and let our highly experienced doctors of TCM help to heal wrist pain naturally.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.
How to Treat Rosacea With Acupuncture and TCM
By Xiaomei Cai, L.Ac., Ph.D. and Qineng Tan, L.Ac., Ph.D.

Facial flushing? Persistent redness, tiny bumps, or a burning sensation across your nose and cheeks? These can be signs of rosacea, a common inflammatory skin condition that affects millions of people. Acupuncture and Traditional Chinese Medicine (TCM) offer holistic rosacea treatment to address both the symptoms and the root causes of rosacea.
What is Rosacea?
Rosacea is a chronic inflammatory skin disease that most often appears in the middle of the face — the nose, cheeks, chin, and forehead. It can cause persistent redness, visible blood vessels, and small, painful pimples or red bumps on skin, like a red dot on face.
While facial rosacea is the most common form, there are some other skin conditions that can be related or sometimes mistaken for rosacea:
Pityriasis Rosea – Though the name is similar, this is actually a different condition caused by a viral infection. It leads to a scaly, pink rash that often appears on the torso and may be mistaken for rosacea, especially in its early stages.
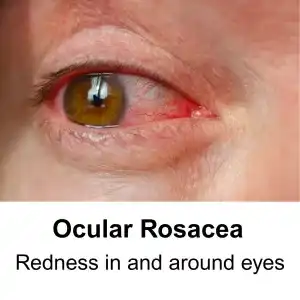
Ocular Rosacea – In some patients, rosacea affects the eyes, causing symptoms like redness or “bloodshot eyes,” burning, stinging, dryness, or a gritty sensation. The eyelids may become inflamed, making the eyes appear bloodshot.
Perioral Dermatitis – considered by some practitioners to be a type of rosacea, this is a face rash that also appears on the face. “Dermatitis” is a general term that covers many types of inflammatory skin conditions.
Rosacea is a chronic skin condition that will flare up at times, and at other times, appear to be improving (remission). If it is left untreated, rosacea can worsen over time and affect other areas, including the eyes.
Acupuncture and TCM can be used as a complementary or alternative treatment for roseacea.
Symptoms of Rosacea
Common signs and symptoms include:
Facial Redness – Persistent redness or flushing, especially across the nose and cheeks.
Visible Blood Vessels – Tiny, broken blood vessels may appear near the surface of the skin.
Acne-like Bumps – Small, red, or pus-filled bumps that can be tender and painful.
Burning or Stinging Sensation – The skin may feel sensitive, warm, or sting when exposed to triggers like sun, wind, or skincare products.
Dry Skin – skin may appear dry, rough, scaly, or thickened (in severe cases).
Eye Symptoms – Red, irritated, or dry eyes (ocular rosacea)
Edema – puffiness or swelling in the face
What Causes Rosacea?
While the exact cause of rosacea is still not fully understood by medical science, many factors may play a role in the development of this skin condition. It is an inflammatory response that may be triggered by the immune system, certain foods, emotional stress, or environmental conditions like sun (U/V rays), heat, or wind. Genetics probably plays a role, as well.
Many people who suffer from rosacea have higher levels of mast cells. Some also have skin mites (Demodex mites). Demodicosis (face mite infestation) is not uncommon, but can show up in increased amounts in people who have rosacea and may be one of the factors that triggers the inflammatory response that contributes to rosacea flare-ups.
SIBO, or intestinal bacterial overgrowth, can sometimes contribute to rosacea.
Rosacea Treatment
A doctor or dermatologist typically diagnoses rosacea based on its characteristic signs and patient history. In some cases, a skin biopsy or other tests might be done to rule out other conditions like lupus or allergic dermatitis.
Common treatments include:
- Topical medications like metronidazole or azelaic acid. Some medications for rosacea constrict blood vessels to reduce redness, while others are antiparasitics
- Retinoids (Vitamin A)
- Oral antibiotics (doxycycline, minocycline) to reduce inflammation
- Laser therapy for visible blood vessels
- Lifestyle and trigger avoidance (avoiding sun exposure, alcohol, spicy foods)
While these treatments can help manage symptoms, rosacea often returns when treatments are stopped, and long-term antibiotic use can affect gut health and immunity.
Can Acupuncture Help Rosacea?

In Traditional Chinese Medicine, rosacea is viewed as a result of internal imbalances that manifest as external skin changes. The skin is seen as an extension of the body’s internal state.
According to TCM theory, rosacea would usually be considered the result of stagnation of Qi, blood, and heat in the body.
Diagnostic patterns that an acupuncturist might observe as being the root cause of rosacea might include:
- Wind-heat of the lung meridian
- Damp heat of spleen and stomach
- Heat stagnation in the liver channel
Heat and toxicity in the lungs and stomach can create excess internal heat, which may rise to the surface, causing redness, flushing, and pustules.
Stagnation of Qi and blood, along with chronic stress, hormonal changes, and dietary habits can impede the flow of qi and blood, leading to stagnation and visible capillaries.
In some patients, dampness combined with heat can cause swelling, acne-like bumps, and increased oiliness.
In long-standing rosacea, depletion of yin (cooling, moistening energy) can cause lingering redness and sensitivity.
How TCM Treats Rosacea
Acupuncture and Traditional Chinese Medicine take a personalized approach to rosacea, focusing on restoring balance within the body and addressing both internal and external symptoms.
Acupuncture works by:
- Reducing systemic and local inflammation
- Improving blood flow and microcirculation
- Regulating the autonomic nervous system
- Helping balance the gut-skin connection
- Calming the body and reducing stress, a common rosacea trigger
Research supports acupuncture as an effective therapy for rosacea. A review and analysis of studies found that a complementary treatment for rosacea combining conventional treatment and TCM therapy reduced the recurrence of symptoms. Acupuncture can reduce flushing, redness, and skin lesions associated with rosacea by modulating inflammatory pathways and promoting tissue healing.
One published case study demonstrated that a patient who had gone through 18 months of conventional treatment for rosacea with unsatisfactory results experience significant improvement after 3 acupuncture treatments, with no recurrence of a flare up in the subsequent six months. Laser Doppler showed increased blood microcirculation (blood flow) in the localized area of the skin rash.
Chinese herbs can be used both internally and externally to reduce redness, clear heat, and support overall skin health. The herbs in one TCM herbal remedy often used to treat rosacea—Liang Xue Wu Hua Tang—for example, works to remove toxins, cool and activate blood, and disperse wind. A traditional formula may be modified to suit the patient’s specific presentation, making TCM highly individualized.
Skincare for Rosacea
In addition to acupuncture and herbs, a TCM practitioner will recommend:
Avoiding rosacea triggers like alcohol, caffeine, and spicy foods.
- Incorporating cooling, anti-inflammatory foods (e.g., leafy greens, cucumber).
- Managing stress and promoting relaxation.
- Maintaining a consistent skincare routine using gentle, hydrating products.
By addressing the root causes of rosacea and working with the body’s natural balance, acupuncture and Traditional Chinese Medicine can help reduce the frequency and severity of rosacea outbreaks, often yielding long-lasting results.
Acupuncture Near Me for Rosacea in West Los Angeles
If you’re tired of dealing with rosacea and want a natural approach that supports both your skin and overall health, we’re here to help. At Art of Wellness Acupuncture, we specialize in treating rosacea and other skin conditions with personalized acupuncture and herbal therapy. Contact us today to book your consultation and take the first step toward calmer, clearer skin.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.
How to Treat Sarcoidosis With Acupuncture and TCM
by Qineng Tan, L.Ac., Ph.D. and Xiaomei Cai, L.Ac., Ph.D.
Fever, fatigue, and muscle aches? Swollen lymph nodes, coughing, shortness of breath? Eye pain, or red eyes? These can all be signs of sarcoidosis, an autoimmune disorder. Acupuncture and TCM can help relieve sarcoidosis symptoms.
Sarcoidosis is a complex autoimmune disease characterized by the formation of granulomas—clumps of inflammatory cells—that can affect multiple organs in the body. It most commonly impacts the lungs and lymph nodes, but it can also involve the skin, eyes, heart, musculoskeletal system, and nervous system.
Sarcoidosis typically manifests in young adults, with the highest prevalence observed in individuals in their 20s and 30s, though it can affect people of any age. This condition’s exact cause remains unknown, but researchers believe it results from an overactive immune response to environmental or infectious triggers.
Sarcoidosis can cause serious and even life-threatening complications, especially when it is centered in the lungs. However, the good news is that many cases of sarcoidosis do eventually clear up or go into remission.
Acupuncture, herbs, and other TCM treatments for sarcoidosis can help address underlying issues that contribute to the formation of this autoimmune disorder, as well has help to relieve symptoms. TCM can also help with potential signs of dysautonomia (autonomic nervous system disorders) that can be caused by sarcoidosis.
Types of Sarcoidosis
There are different types of sarcoidosis depending on which organs are affected.
Pulmonary sarcoidosis, which targets the lungs, is the most common form and can lead to chronic respiratory issues.
Musculoskeletal sarcoidosis may cause joint inflammation (arthritis), muscle pain, or bone lesions, sometimes resulting in long-term complications such as osteoporosis.
Sarcoidosis can lead to vascular complications that involve inflammation of small, medium, or large blood vessels. These types of sarcoid-related vasculitis are rare but important to recognize, as they may present with overlapping features of other autoimmune or vascular conditions.
Small-vessel vasculitis in sarcoidosis primarily affects the skin. This type of vasculitis might coexist with sarcoidosis and manifests as petechiae (small red or purple spots on the skin), purpuric spots (purple “blood spots” under the skin, due to broken blood vessels), or infiltrative erythema (raised rash, like welts on skin).
Medium-vessel sarcoid vasculitis often involves pulmonary lymphatic capillaries and may present with systemic symptoms, including fever, arthritis, and cutaneous manifestations (skin rash or lesions).
Sarcoidosis symptoms can vary widely but may include persistent fatigue, fever, shortness of breath, coughing, swollen lymph nodes, and joint pain. Because of its wide range of manifestations, sarcoidosis can be difficult to diagnose and often requires imaging tests, biopsies, and bloodwork.
New Diagnostic Methods for Sarcoidosis

Diagnosing sarcoidosis remains a complex challenge for clinicians because there is no single definitive test for the disease. The diagnosis is often made by combining a thorough clinical evaluation, imaging studies, laboratory tests, and biopsy results. However, emerging research has identified new biomarkers that may help streamline the diagnostic process.
One promising development involves the discovery of type 1 innate lymphoid cells (ILC1) as a potential biomarker for sarcoidosis. A study led by researchers at the University of Pennsylvania compared skin samples from sarcoidosis patients to those with granulomas caused by other conditions. They found that levels of ILC1 were significantly higher in sarcoidosis-affected tissues. This trend was also observed in lung granulomas and even in the bloodstream, where sarcoidosis patients showed a 12-fold increase in circulating ILC1 levels compared to healthy individuals.
Sarcoidosis Treatment
The main goals of treatment for sarcoidosis are managing symptoms, reducing the risk of organ damage, and improving the patient’s quality of life. In some cases, sarcoidosis may go into remission, meaning that the condition is no longer causing complications.
Patients with mild or no symptoms might not require treatment, just monitoring. When treatment is necessary, Western medicine focuses on reducing inflammation and suppressing the overactive immune system. These treatments can be highly effective but often come with potential risks and side effects.
Prednisone is usually the first-line treatment for sarcoidosis. This steroid medication suppresses the immune system and reduces inflammation, which can help to improve symptoms and prevent organ damage. However, long-term use of prednisone may lead to significant side effects, such as weight gain, bone loss, high blood sugar, and an increased risk of infection. For this reason, corticosteroid doses are typically tapered once symptoms improve, or alternative medications may be introduced to minimize steroid use.
Methotrexate, a drug commonly used for severe rheumatoid arthritis, is another option for managing sarcoidosis. It is particularly effective in patients with significant organ involvement, such as lung, skin, or joint manifestations. Methotrexate helps to suppress the immune system and can be used in combination with corticosteroids to reduce the need for higher steroid doses.
Drugs such as hydroxychloroquine, which are typically used to treat malaria, can be effective for sarcoidosis that primarily affects the skin or joints. These medications may also be helpful for managing chronic fatigue and muscle pain associated with the condition.
Tumor necrosis factor (TNF) inhibitors, like infliximab or adalimumab, are biologic medications that help reduce inflammation. These drugs are often used in patients with severe sarcoidosis, particularly when other treatments have not been effective. TNF inhibitors can be administered intravenously or as an injection under the skin.
Corticotropin is a medication that stimulates the adrenal glands to produce natural steroid hormones. It can be injected under the skin to help manage inflammation and reduce immune system activity, offering an alternative to synthetic corticosteroids.
Acupuncture and other TCM treatments can be helpful for clearing inflammation and relieving symptoms related to sarcoidosis, as well as helping to manage the side effects that may be caused by other medications.
Can Acupuncture Help Sarcoidosis?

In TCM, sarcoidosis is viewed as a condition arising from underlying imbalances in the body. These imbalances are often associated with heat, phlegm, and stagnation of Qi and blood. Granulomas, for example, may be interpreted as accumulations of dampness and phlegm obstructing the free flow of Qi and blood. Furthermore, the systemic inflammation seen in sarcoidosis can be attributed to excessive heat in the body. TCM practitioners focus on identifying the root causes of these imbalances and tailoring treatments to the individual’s unique presentation.
Acupuncture treatments for sarcoidosis aim to reduce inflammation, support the immune system, and restore balance within the body. By stimulating specific acupuncture points, practitioners can promote the smooth flow of Qi and blood, reduce stagnation, and clear heat and dampness. This can help alleviate symptoms such as shortness of breath, fatigue, and joint pain, which are commonly experienced by those with sarcoidosis.
Research has shown that acupuncture can help modulate the immune system, reduce stress, and improve quality of life for people with chronic inflammatory conditions. For sarcoidosis patients, regular acupuncture sessions may not only provide symptom relief but also address the underlying imbalances contributing to the disease.
Chinese Medicine diagnosis is different from Western medicine diagnosis. An acupuncture practitioner will look carefully at each individual patient’s specific symptoms, medical history, and foundational constitution to discover the underlying causes of their particular presentation of disease.
In the case of sarcoidosis, possible TCM diagnoses might be:
- Lung Qi Deficiency – presents with symptoms like shortness of breath, weak lung sounds, throat rattling, spontaneous sweating, feeling cold, pale complexion, weak voice. Treatment will seek to tonify Lung Qi to strengthen respiratory function possibly with the inclusion of moxibustion treatment.
- Lung Yin Deficiency – symptoms: breathlessness, night sweats, 5-center heat (warmth in palms, soles, and chest), dry throat, non-productive cough, malar flush, red skin lesions. Treatment goals include nourishing Lung Yin and clearing heat.
- Lung Qi Stagnation – symptoms: chest congestion/blockage, difficulty breathing, emotional grief or melancholy, trouble letting go of the past, and constipation. Treatment will help improve circulation of Lung Qi to relieve stagnation and promote emotional well-being.
- Phlegm in the Lungs- symptoms: Chronic phlegm retention contributing to fibrous tissue and scarring, which can parallel conditions such as chronic bronchitis. There may also be phlegm-related symptoms like congestion or rattling breath. Treatment will seek to nourish Lung Qi, transform phlegm, and circulate Qi to reduce stagnation.
These differential diagnoses reflect the diverse ways in which TCM approaches pulmonary dysfunctions and can be used to tailor treatments for individuals with sarcoidosis, ensuring that the root causes and symptoms are addressed holistically.
Acupuncture for Sarcoidosis Near Me in West Los Angeles
If you or someone you know is suffering with sarcoidosis, or perhaps has some of the symptoms mentioned above, but has not been able to get adequate diagnosis or treatment for their condition, it may be appropriate to seek care from a qualified TCM doctor. Dr. Tan and Dr. Cai at Art of Wellness in Los Angeles, just east of Santa Monica, have over 35 years of experience helping people with all types of autoimmune disorders, skin conditions, respiratory problems, and musculoskeletal pain. We can help you find relief and better health.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.
How to Treat Wrist Pain With Acupuncture and TCM
By Qineng Tan, L.Ac. Ph.D. and Xiaomei Cai, L.Ac., Ph.D.

Wrist pain when you bend it? Is it hard to open jars or doors? Popping sound in wrist? Pain at the base of the thumb? Wrist or fingers swollen? Wrist pain can be caused by a variety of joint issues, including tendinitis of wrist, or De Quervain’s tenosynovitis. Acupuncture and TCM can help treat the root cause of wrist pain.
The wrist is a complex joint composed of several small bones, tendons, ligaments, muscles, and nerves. In medical terminology, the thumb side of the wrist is the radial wrist (wrist pain on thumb side, radial thumb pain, or inner wrist pain), while the little finger side is the ulnar wrist (wrist pain on pinky side, ulnar wrist pain, or outer wrist pain).
Injuries, such as a wrist fracture, are a particularly common cause of acute wrist pain, as people will often try to catch themselves with an outstretched hand when falling, which can easily lead to wrist injury. Wrist fractures can result in wrist pain, swelling, bruising, and an inability to move the wrist normally.
Fractures may also damage nearby ligaments, nerves, and tendons, which can complicate healing and prolong discomfort. Proper alignment and stabilization are essential for healing, and if not treated correctly, a fracture can lead to chronic pain and arthritis in the wrist.
Acupuncture treatment can certainly be helpful for reducing inflammation, relieving acute pain, and helping to speed the healing of a wrist fracture.
Other, more chronic conditions can also cause wrist pain.
Top 5 Causes of Wrist Pain
Certain chronic health conditions that build up slowly over time can ultimately lead to wrist pain and dysfunction. Some of these include:
- Arthritis of the Wrist – Osteoarthritis of the wrist and rheumatoid arthritis can both be causes of wrist pain. Osteoarthritis is typically caused by wear and tear on the cartilage of the wrist joint. This condition usually develops slowly over time, especially in individuals who have experienced previous injuries or repetitive stress on the wrist. Rheumatoid arthritis is an autoimmune condition that causes inflammation of the wrist joints, leading to pain, warmth, and eventual joint damage. Both types of arthritis can severely limit the range of motion and strength in the wrist, making even simple activities painful.
- Repetitive Stress Injury (RSI) – Repetitive stress injuries in the wrist are caused by continuous or repetitive movements, such as typing, gripping, or lifting, which can strain the tendons and ligaments in the wrist. Over time, this repetitive strain can lead to inflammation, pain, and decreased mobility. Carpal tunnel syndrome and tendonitis (discussed further below) are common forms of repetitive strain injury that cause wrist pain. RSI often requires rest and modification of activities to allow the wrist to heal, as continuous stress can worsen the condition and lead to long-term issues.
- De Quervain’s Tenosynovitis – De Quervain’s tenosynovitis (also known as Quervain disease or styloid tenosynovitis) affects the tendons on the thumb side of the wrist. It occurs when the tendons around the base of the thumb become inflamed, leading to pain and tenderness, particularly during movements that involve gripping or pinching. This condition is often the result of repetitive thumb movements, such as those used in typing or texting. De Quervain’s disease tenosynovitis can cause sharp pain on the radial (thumb) side of the wrist, and people may find it difficult to grasp or hold objects.
- Tendonitis (or Tendinitis) of the Wrist – Tendonitis of the wrist refers to inflammation of the tendons that cross the wrist joint. It is commonly caused by repetitive motion, excessive strain, or sudden injury. Tendonitis can affect various tendons depending on the type of movement that led to the condition. Pain and swelling are typical symptoms, and the affected area may feel warm to the touch. Wrist tendonitis is often seen in athletes and individuals who perform repetitive tasks with their hands and can result in decreased wrist function and grip strength.
- Carpal Tunnel Syndrome – Carpal tunnel syndrome is a type of neuropathy, or nerve pain, caused by compression of the median nerve as it passes through the carpal tunnel in the wrist. This compression leads to pain, tingling, numbness, and weakness in the hand and wrist. Carpal tunnel syndrome is often associated with repetitive wrist movements and can be exacerbated by activities that involve gripping or bending the wrist. If left untreated, carpal tunnel syndrome can lead to permanent nerve damage and reduced hand function.
Other possible causes of wrist pain could include: bursitis (small, fluid-filled sacs that form between bones), ganglion cysts (fluid-filled cysts that form near joints), or Kienbock’s disease (in which the lunate bone of the wrist begins to break down).
Treatment for Wrist Pain
When a patient presents with wrist pain, diagnosis usually begins with a physical examination to identify the specific cause of pain. The doctor will assess the patient’s range of motion, grip strength, and any areas of tenderness or swelling in the wrist. Imaging via X-rays, MRI or ultrasound may be used to confirm a diagnosis, especially if a fracture, ligament tear, or nerve compression is suspected.
For nerve-related issues like carpal tunnel syndrome, a nerve conduction study (NCS) or electromyography (EMG) may be conducted to assess the functionality of the median nerve. This can help differentiate between arthritis, repetitive strain injuries, or specific tendon and nerve issues.
Conventional treatments for wrist pain depend on the specific diagnosis. In cases of arthritis, anti-inflammatory medications (NSAIDs), corticosteroid injections, or physical therapy are commonly recommended to manage pain and improve joint mobility.
For fractures, immobilization with a cast or splint is typically required, and surgery may be necessary for more severe breaks. Repetitive stress injuries like tendonitis or De Quervain’s tenosynovitis often respond to rest, ergonomic modifications, and anti-inflammatory treatments.
Physical therapy exercises to strengthen and stretch the affected muscles and tendons can be helpful. In cases of carpal tunnel syndrome, wrist splints are often used to keep the wrist in a neutral position, particularly at night, and corticosteroid injections may be administered, aimed to reduce inflammation.
If these methods do not relieve symptoms, surgical intervention, such as carpal tunnel release, might be recommended to decompress the median nerve.
While typical treatment usually involves pain medication, rest, and possibly physical therapy, acupuncture treatment can be an excellent adjunct or alternative treatment to relieve wrist pain.
Can Acupuncture Help Wrist Pain?

Acupuncture and Traditional Chinese Medicine (TCM) can offer natural pain relief for injuries and chronic pain conditions, by reducing pain and inflammation, improving circulation, and supporting the body’s healing process.
According to TCM theory, the health of the internal organ systems is related to the rest of the body parts. For example, the spleen is responsible for transforming Qi and blood. If the spleen is weak, it can cause blockages in blood flow that create stasis, stiffness and pain in the limbs and joints. The liver governs the tendons of the body. When the liver is not functioning well, often due to emotional stress, than there may be pain and dysfunction in the tendons and joints.
Therefore, an acupuncturist does not only treat the painful area, but also looks at the deeper root cause and addresses them with acupuncture treatment, Chinese herbs, and other therapeutic modalities, to help relieve pain and inflammation and bring about healing.
A systematic review of trials showed that acupuncture treatment led to significant pain reduction for patients treated for rheumatoid arthritis affecting the wrist. It also concluded that acupuncture brought about pain relief and functional improvement for patients with tenosynovitis and carpal tunnel syndrome.
One study separated patients with carpal tunnel syndrome into two groups: one group received pain medication for wrist pain and the other group had 12 acupuncture treatments. Comparatively, the acupuncture group had greater reduction in pain, tingling, and numbness and greater functional improvement.
Studies of MRI results after acupuncture have suggested that acupuncture for carpal tunnel syndrome actually has a positive impact on nerve function in the wrist and changes the way the brain and nerves are signaling pain.
A trial involving patients treated for De Quervain’s disease tenosynovitis with five acupuncture sessions over the course of two weeks showed improvement in pain and grip strength, and the results were still maintained at a ten week follow up visit.
The combination of acupuncture and moxibustion can be particularly helpful for treating Quervain’s tenosynovitis.
Overall, the evidence shows that acupuncture and other TCM modalities can be a relatively low cost, non-invasive way of helping to treat wrist pain, without surgery or the unwanted side effects of pain medications or steroid injections.
Acupuncture Near Me for Wrist Pain in Los Angeles
Dr. Tan and Dr. Cai at Art of Wellness in West L.A. have over 35 years of experience helping people recover from sports injuries, repetitive stress injuries, and orthopedic pain conditions of all kinds. Acupuncture treatment for wrist pain can be used in addition to your medical protocol to help speed recovery and bring about pain relief.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.
How to Treat Cervical Radiculopathy With Acupuncture and TCM
By Qineng Tan, L.Ac., Ph.D. and Xiaomei Cai, L.Ac., Ph.D.
Neck pain? Stiff neck? These could be signs of cervical radiculopathy caused by a pinched nerve in neck. Acupuncture and TCM can provide neck pain relief and address the underlying causes of cervical radiculopathy.
Cervical radiculopathy occurs when a nerve in the neck becomes compressed or irritated where it branches away from the spinal cord. This is often referred to as a “pinched nerve.” This condition can lead to neck pain, weakness, and other symptoms not only in the neck but radiating into the arms and hands as well.
Cervical radiculopathy can be caused by several different factors, most of which involve some form of nerve compression in the neck.
One of the most common causes is a herniated disc, also known as a slipped disc in neck, or bulging disc in neck. This happens when the gel-like center of a spinal disc pushes out through a crack in the tougher exterior, putting pressure on a nearby nerve root. This can happen due to injury or degeneration over time.
Cervical spondylosis, also known as neck arthritis or cervical osteoarthritis, is a common age-related condition that affects the joints and discs in your neck. As the discs and cartilage between the cervical vertebrae wear down, this can cause neck pain and stiffness.
Degenerative disc disease and osteoarthritis are also common causes of a pinched nerve in neck. As we age, the spinal discs lose water content and shrink, leading to decreased cushioning between the vertebrae. This can cause the bones to rub against each other and lead to the formation of bone spurs, which can press on nerves and cause radiculopathy.
Another potential cause is spinal stenosis, which is the narrowing of the spaces within the spine. Lumbar spinal stenosis can result from a variety of factors, including thickened ligaments or overgrown bones, and leads to pinching or compression of the nerve roots as they exit the spinal column.
Additionally, trauma or injury to the neck, such as from car accidents or sports injuries, can directly damage the vertebrae or discs and result in a pinched nerve.
In more rare cases, tumors or infections in the spine may also cause cervical radiculopathy by compressing nerve roots.
Top 5 Symptoms of Cervical Radiculopathy
Pain in the neck and shoulders and headache are the most common symptoms associated with cervical radiculopathy. Poor reflexes and muscle weakness can also occur with a pinched nerve in the neck.
- Neck and shoulder pain – sharp or burning pain that starts in the neck and may radiate down the shoulder, arm, and hand
- Neck Stiffness – difficulty turning or moving the neck, neck muscle pain, muscle spasm in neck
- Numbness or Tingling in the shoulder, arms, or hands due to nerve compression.
- Muscle weakness in the arms or hands, trouble gripping or lifting objects.
- Neck pain and headache, headache that starts with neck pain
Diagnosis and Treatment for Cervical Radiculopathy
Diagnosing cervical radiculopathy can be challenging because its symptoms—such as neck pain, numbness, or tingling radiating down the arm—can overlap with other conditions like muscle strain, carpal tunnel syndrome, or even heart problems.
The complexity of nerve pathways makes it difficult to pinpoint the exact location and cause of nerve compression based on symptoms alone. The pain can vary in intensity, and some patients may not experience obvious arm symptoms, leading to confusion in initial assessments.
Western medicine typically relies on a combination of clinical evaluation and diagnostic imaging to confirm cervical radiculopathy.
During the clinical evaluation, a doctor will perform a physical examination, testing the strength, reflexes, and range of motion in the neck and arms. A Spurling’s test, where the head is turned and pressure is applied to the top of the head, may be used to reproduce symptoms and help localize the nerve root affected.
To confirm the diagnosis, imaging studies such as X-rays, CT scans, or MRIs are often used to visualize the spine and detect any structural issues, like herniated discs or bone spurs, that could be compressing the nerve roots. An electromyography (EMG) or nerve conduction study may also be performed to assess how well the nerves are functioning and to rule out other conditions affecting nerve function.
Conventional treatments for cervical radiculopathy, or treating a pinched nerve, generally focus on reducing pain, managing inflammation, and restoring normal function.
NSAID medications like ibuprofen or naproxen are usually recommended to reduce pain and inflammation around the pinched nerve. Corticosteroid injections may be used to reduce inflammation around the nerve root and offer temporary relief. Muscle relaxers may be prescribed to ease muscle spasms and reduce pressure on the pinched nerve.
Physical therapy exercises designed to improve neck mobility and strengthen supporting muscles, can potentially help relieve nerve compression. Using cervical traction devices to gently stretch the neck and reduce pressure on the affected nerve may be helpful in some cases.
In severe cases where non-surgical treatments don’t work, surgical options may be recommended to relieve pressure on the nerve by removing or repairing the affected disc or vertebra.
Acupuncture can be an effective modality for treating neck pain and stiffness due to cervical radiculopathy, without the unwanted side effects of taking pain medications and muscle relaxants.
Can Acupuncture Help Cervical Radiculopathy?

Acupuncture offers an alternative for patients suffering from neck pain who want to avoid surgery and the side effects of medication. Acupuncture treatment stimulates the body’s natural healing processes and alleviates pain by influencing the nervous system, reducing inflammation, and improving blood circulation to affected areas.
Acupuncture functions in multiple ways to help relieve nerve compression pain. It can help reduce swelling, or edema, that contribute to nerve compression. It also helps to relax muscle spasms. Acupuncture helps to increase blood flow to nerve roots.
Studies have shown that acupuncture can yield favorable outcomes, often comparable to conventional drug therapies. For instance, one randomized clinical trial found that acupuncture provided similar pain relief to drug therapy, making it a viable, safer alternative for pain management in cervical radiculopathy patients.
Additionally, some research has demonstrated the benefits of combining acupuncture with other conservative treatments, like cervical manipulations, to enhance therapeutic outcomes. In clinical trials, this combination has proven effective in reducing pain and improving mobility.
Acupuncture, used to complement other modalities, can be used as a valuable tool in the management of cervical radiculopathy, offering an effective, low-risk option to relieve pain and restore better mobility.
One case study of a patient with a C6/7 disc prolapse and radiculopathy showed that over a course of six acupuncture sessions administered within four weeks, significant improvements were observed in both pain and range of motion. Pain levels dropped from 8/10 to 2/10.
Acupuncture Near Me for Cervical Radiculopathy in West L.A.
At Art of Wellness Acupuncture and TCM in West Los Angeles, we have over 35 years of experience helping people find relief from all types of pain conditions related to nerve compression and neck pain, including herniated disks, spinal stenosis, cervical spondylosis, and cervical radiculopathy. Dr. Tan and Dr. Cai provide specialized care for each individual patient, including herbal remedies, therapeutic Chinese massage, and electroacupuncture to help relieve pain.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.