-
 Art of Wellness Acupuncture & Traditional Chinese Medicine (TCM)11704 Wilshire Blvd, Suite 295, Los Angeles, CA, 90025
Art of Wellness Acupuncture & Traditional Chinese Medicine (TCM)11704 Wilshire Blvd, Suite 295, Los Angeles, CA, 90025
myartofwellness@gmail.com310-451-5522 Office Hours
MonClosedTue7:30 am --4 pmWed7:30 am --4 pmThu7:30 am -- 4 pmFri7:30 am -- 4 pmSat7:30 am -- 4 pmSunClosedOur office opens from Tuesdays to Saturdays 7:30 am to 4 pm, will be closed on Memorial day, Independent day, Labor day, Thanksgiving day, Christmas and New year.
-
Recent Posts
- How to Treat De Quervain’s Tenosynovitis With Acupuncture and TCM
- Chinese New Year 2026: Year of the Horse
- Acupuncture and TCM Treatment for Perimenopause Symptoms
- How to Treat Insulin Resistance With Acupuncture and TCM
- How to Treat Metabolic Syndrome With Acupuncture and TCM
- How to Treat Syncope With Acupuncture and TCM
- How to Treat Thoracic Outlet Syndrome With Acupuncture and TCM
- How to Treat Dupuytren’s Contracture With Acupuncture and TCM
- How to Treat Nutcracker Syndrome With Acupuncture and TCM
- How to Treat Rosacea With Acupuncture and TCM
- How to Treat Perioral Dermatitis With Acupuncture and TCM
- Lymphatic Drainage With Acupuncture and TCM
- How to Treat Turf Toe With Acupuncture
- How to Treat Nerve Pain With Acupuncture and TCM
- How to Treat Watery Eyes With Acupuncture and TCM
- How to Treat Ovarian Cysts With Acupuncture and TCM
- Sign up to receive news and updates and get my free report:“The Top 10 Reasons to Try Acupuncture”

December 2025 M T W T F S S 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31
Uncategorized
Lymphatic Drainage With Acupuncture and TCM
By Xiaomei Cai, L.Ac., Ph.D. and Qineng Tan, L.Ac., Ph.D.
Persistent swelling in your arms, legs, or other areas of your body? This could be a sign of lymphedema, a condition caused by the buildup of lymphatic fluid. Acupuncture and Traditional Chinese Medicine (TCM) offer a gentle and effective way to promote lymphatic drainage and support the body’s natural detoxification process.
What Is Lymphedema?
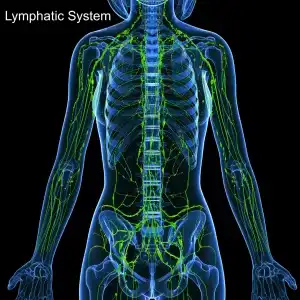
The lymphatic system is a complex network of nodes, tubes and ducts that move lymph fluid through the body, carrying immune cells (like T cells, B cells, and NK cells) that fight against bacteria, viruses, cancer cells, and damaged cells.
Lymphedema is a chronic condition that occurs when the lymphatic system is unable to properly drain lymph fluid, leading to fluid retention and tissue swelling. When the system is blocked or damaged, lymph can accumulate in the tissues, causing swelling and discomfort.
Top 10 Symptoms of Lymphedema
Signs of lymphedema, or lymphatic edema, can develop slowly over time or come on quite suddenly. At first, you may notice that a part of your body is a little swollen, or that your arm or leg just seems a little bit more swollen and stiff than the other one. Your clothes might seem a little bit tighter.
You might notice that you can’t see veins in your limbs, when you used to be able to. Your joints just may seem stiff. It can be easy to attribute mild symptoms of lymphedema to hot weather, general inflammation, or simply aging.
As lymphedema progresses to more severe stages, you may begin to notice that the affected areas are always stiff and swollen, firm to the touch, and that the skin in those areas is becoming noticeably thicker.
Common symptoms of lymphedema include:
- Swelling in the arms, legs, fingers, toes, face, or trunk
- A feeling of heaviness or tightness in the affected area, restricted range of motion
- Aching or discomfort in the swollen limb
- Recurring infections in the affected area
- Hardening or thickening of the skin (fibrosis), redness, itchy skin, rosacea
Symptoms of lymphedema may worsen over time if they are not addressed. Acupuncture and TCM offer a holistic way to treat lymphedema and manage the underlying conditions that cause swelling.
Common Causes of Lymphedema
There can be many different factors that lead to a buildup of lymphatic fluid. A few of the most common causes of lymphatic edema include:
- Surgical removal of lymph nodes (commonly due to cancer treatment)
- Radiation therapy that damages lymph vessels or nodes
- Infections that cause inflammation and blockage of lymphatic vessels
- Cancer that spreads to or blocks lymph nodes
- Injury or trauma to the lymphatic system
- Congenital malformations or underdeveloped lymphatic vessels (primary lymphedema)
- Obesity and sedentary lifestyle that impair lymph flow
Treatment for Lymphedema

Conventional treatment for lymphedema typically focuses on symptom management and improving quality of life. This may include a recommendation to wear compression garments like sleeves or stockings to encourage lymph flow. Manual lymphatic drainage (MLD): A specialized massage technique performed by trained therapists to move lymph fluid manually.
Gentle, regular physical activity may be recommended to help stimulate lymphatic circulation.
Machines known as Pneumatic compression devices, such as inflatable sleeves worn on the limbs, can mimic manual drainage.
In some cases, procedures to remove excess tissue or improve drainage pathways.
While these methods can help manage the symptoms, they often need to be maintained consistently and may not address the underlying systemic imbalances.
TCM View of Lymphedema
In Traditional Chinese Medicine, lymphedema is viewed as a disruption of the body’s natural flow of Qi (vital energy) and fluids. According to TCM theory, the spleen plays a central role in fluid metabolism. When the spleen Qi is weak or deficient, it cannot properly transform and transport fluids, leading to dampness and phlegm accumulation. This internal dampness can settle in the limbs and cause swelling.
Lymphedema may also be related to stagnation of Qi and blood, particularly in the channels (meridians) that traverse the affected area. External factors like trauma, surgery, or radiation can block the flow of Qi and blood, creating what TCM refers to as “blood stasis.”
Key TCM patterns that may contribute to lymphedema include:
- Spleen Qi deficiency
- Damp accumulation
- Qi stagnation
- Blood stasis
Can Acupuncture Help With Lymphatic Drainage?

Acupuncture helps to regulate the flow of Qi and blood through the meridians. When specific points are stimulated, they can promote circulation and encourage the movement of stagnant fluids.
Herbal medicine and acupuncture treatments can strengthen the spleen’s function of fluid transformation and transport. Strengthening the kidneys also helps resolve chronic dampness and supports the body’s ability to detoxify.
Research has shown that acupuncture has anti-inflammatory and analgesic effects. For patients experiencing pain, heaviness, and aching due to lymphedema, acupuncture can provide relief.
A healthy lymphatic system is essential for immune function. Acupuncture has been found to modulate immune activity and may help reduce the frequency of infections associated with lymphedema.
Gentle massage techniques like Tui Na and Gua Sha can be applied along the meridians to manually stimulate lymphatic drainage. Unlike deep tissue massage, these methods work with the body’s energy system to promote gentle, effective movement of fluids without overwhelming the tissues.
One study of women who had breast cancer related lymphedema found that twice weekly acupuncture sessions over the course of four weeks helped reduce swelling in their arms.
A review of studies on acupuncture treatment for cancer patients showed that acupuncture not only helped with lymphatic swelling, but also helped to relieve anxiety and depression, nausea and vomiting, and chemotherapy induced neuropathy.
Acupuncture Near Me for Lymphatic Drainage in West Los Angeles
Lymphedema can be a chronic and frustrating condition, but there are holistic options that go beyond symptom management. Acupuncture and TCM offer time-tested methods to support lymphatic drainage, strengthen the body’s natural detox systems, and relieve discomfort. If you’re living with lymphedema or chronic swelling, reach out to us at Art of Wellness Acupuncture in West Los Angeles. We’d be happy to create a personalized treatment plan to help you feel lighter, more comfortable, and more energized again.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.
How to Treat Turf Toe With Acupuncture
By Qineng Tan, L.Ac., Ph.D. and Xiaomei Cai, L.Ac., Ph.D

Do you have pain in your big toe when you put weight on it or press on it? Swelling at the base of the big toe, bruising, or inflammation in the big toe? These can be signs of “turf toe,” or a sprained big toe joint. Acupuncture and TCM offer an alternative treatment for turf toe pain.
Turf toe is a common yet often underestimated injury that can have a serious, negative impact on your sports performance and daily life. Characterized by pain at the base of the big toe, this condition results from a sprain of the metatarsophalangeal (MTP) joint.
Turf toe pain is a serious problem for professional athletes, but it can affect anyone. Big toe pain can plague every step you take throughout your day.
While conventional treatments for turf toe typically focus on rest and rehabilitation, acupuncture and Traditional Chinese Medicine (TCM) offer complementary approaches that address both symptoms and underlying imbalances and help speed healing.
What Causes Turf Toe?
Turf toe occurs when the big toe is forcibly bent upward, overstretching or tearing the soft tissues around the MTP joint. This injury is especially common among athletes who play on artificial turf, hence the name “turf toe.”
Turf toe injuries can happen when you play football, soccer, basketball, or gymnastics—any type of physical activity that requires you to push off your toes to sprint or spring, lifting the heel high off the ground in such a way that the big toe bends with force involved.
The rigid surface of turf fields, combined with flexible footwear, increases the risk of hyperextension injuries. Any kind of activity that involves sudden starts, stops, and directional changes can possibly contribute to a turf toe injury.
Top 5 Symptoms of Turf Toe
Signs that your big toe pain may be due to turf toe may include:
- Pain at the base of the big toe
- Swelling and bruising around the big toe joint
- Limited range of motion
- Tenderness when pressing on the toe
- Difficulty bearing weight or pushing off the foot
You may have a feeling of instability around the base of the toe joint. Turf toe symptoms may occur suddenly after a particular movement, or they can build up gradually over time, due to repetitive stress.
Acupuncture provides a holistic alternative or complementary treatment for turf toe. By stimulating specific points on the body, acupuncture aims to reduce inflammation, alleviate pain, and promote healing.
Diagnosis and Treatment for Turf Toe

In Western medicine, turf toe is diagnosed through a combination of physical examination and imaging studies, such as X-rays or MRIs, to assess the extent of soft tissue damage.
Medical treatment for turf toe typically follows the RICE protocol:
- Rest
- Ice
- Compression
- Elevation
Nonsteroidal anti-inflammatory drugs (NSAIDs) may be prescribed to manage pain and swelling. In more severe cases, immobilization with a boot or brace is recommended, and physical therapy may be initiated to restore strength and flexibility. Surgical intervention is rare and reserved for cases where conservative treatments are not helping alleviate pain or improve the proper functioning of the toe joint.
Can Acupuncture Help Turf Toe?
Traditional Chinese Medicine views turf toe not merely as a localized injury but as a manifestation of imbalances within the body’s energy systems. According to TCM, the liver and spleen meridians traverse the area of the big toe. An injury like turf toe can disrupt the flow of Qi (vital energy) and blood along these meridians, leading to pain, swelling, and impaired function.
TCM treatment aims to restore balance and promote healing by:
- Stimulating acupuncture points along affected meridians to enhance Qi and blood flow
- Reducing inflammation and alleviating pain
- Strengthening the body’s innate healing mechanisms
Herbal remedies and other modalities like moxibustion may also be incorporated to support recovery.

One review of studies related to acupuncture for sports injuries concluded that acupuncture can be a good alternative or adjunct treatment for pain relief. Acupuncture can help, so that a person does not become overly dependent on pain medications and steroids, which can have negative side effects. Acupuncture also reduces overall inflammation that can affect other parts of the body.
TCM and acupuncture offer holistic treatment that takes the whole person into account. When athletes suffer an injury, they not only require healing in the specific body part that is affected. They need to undergo healing on a physical, mental, and emotional level in order to get back into the game with confidence.
Acupuncture can also help people who are coming back from an injury with feelings of anxiety and other mental and emotional difficulties, as well as helping to bring all organ systems back into balance.
Acupuncture Near Me for Turf Toe in West Los Angeles
Turf toe can be a debilitating condition that hampers mobility and athletic performance. While conventional treatments focus on symptom management, acupuncture and TCM offer a comprehensive approach that addresses the root of the problem. By restoring balance and promoting the body’s natural healing processes, acupuncture can be an effective option for those seeking relief from turf toe.
If you’re experiencing big toe pain or suspect you have turf toe, consider scheduling a consultation with Art of Wellness Acupuncture in West Los Angeles. Our experienced practitioners can develop a personalized treatment plan to help you return to your active lifestyle.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.
How to Treat Nerve Pain With Acupuncture and TCM
By Qineng Tan, L.Ac., Ph.D. and Xiaomei Cai, L.Ac., Ph.D.
Struggling with sharp, burning, or tingling pain? Do your hands or feet feel numb or hypersensitive? Nerve pain—also called neuropathic pain—can be relieved with acupuncture treatment and other TCM modalities.
Nerve pain occurs when nerves are damaged or dysfunctional, sending incorrect pain signals to the brain. Unlike pain caused by injury or inflammation, nerve pain can persist without an obvious cause and may not respond well to common pain relievers.
Nerve pain can interfere with your ability to work, sleep, or enjoy your day-to-day life. The good news is that acupuncture can be an effective way to treat nerve pain.
What Causes Nerve Pain?
There are many possible underlying conditions that can lead to nerve pain. Here are some of the 10 most most common causes of nerve pain:
- Peripheral neuropathy – often due to diabetes, chemotherapy, or alcohol use
- Trigeminal neuralgia – intense facial pain due to nerve irritation
- Occipital neuralgia – shooting pain at the back of the head and neck
- Cervical radiculopathy – pinched nerves in the neck causing radiating pain
- Carpal tunnel syndrome – pressure on the median nerve in the wrist
- Spinal stenosis or Lumbar stenosis – narrowing of the spinal canal that compresses nerves
- Sciatica – pain radiating down the leg due to sciatic nerve irritation
- Postherpetic neuralgia – lingering nerve pain after shingles
- Dystonia and other movement disorders – can involve nerve dysfunction
- Multiple sclerosis and other autoimmune diseases – affecting nerve conduction
Medical Treatment for Nerve Pain

In Western medicine, the diagnostic process for nerve pain typically begins with a detailed health history and physical examination, focusing on neurological function. Physicians may conduct reflex tests, strength assessments, and evaluate your sensory response. Imaging tests such as MRI or CT scans can help identify structural causes like herniated discs or spinal stenosis. Nerve conduction studies and electromyography (EMG) may be used to assess how well the nerves and muscles are functioning.
Once nerve pain is diagnosed, treatment often involves medications aimed at disrupting the abnormal pain signals. Doctors may prescribe anticonvulsant drugs like gabapentin or pregabalin, which were originally developed to treat epilepsy but are now commonly used to relieve nerve pain.
Certain antidepressants, such as amitriptyline or duloxetine, are also frequently used—not for their mood-enhancing effects, but because they influence how the nervous system processes pain. In some cases, opioids may be prescribed, though they are generally considered a last resort due to the risk of dependence and side effects.
Topical treatments like lidocaine patches or capsaicin cream may offer localized relief for some people. Corticosteroid injections may be recommended if inflammation is contributing to nerve compression, such as in cases of radiculopathy or carpal tunnel syndrome.
Physical therapy can be useful for improving strength, mobility, and nerve function, especially when musculoskeletal imbalances are part of the problem. In more severe cases—such as when a nerve is severely compressed or damaged—surgical intervention may be considered.
While these treatments can sometimes provide temporary relief, they may not address the root cause of nerve dysfunction. Additionally, many patients find that medications come with undesirable side effects or offer only partial relief. That’s why more and more people are turning to acupuncture and Traditional Chinese Medicine (TCM) as a complementary or alternative solution for managing nerve pain holistically.
Can Acupuncture Help Nerve Pain?

In the Western medical model, nerve pain—also called neuropathic pain—is typically understood as the result of damage or dysfunction within the nervous system. This could be due to injury, chronic conditions like diabetes, infections such as shingles, or musculoskeletal issues like spinal stenosis or herniated discs.
TCM, on the other hand, views nerve pain through a holistic lens, focusing on the flow of energy—known as Qi—through the body’s channels or meridians. In this system, pain is often caused by Qi and blood stagnation, which leads to blockages along these pathways. This stagnation can arise from a deficiency in the liver or kidney systems, which in TCM are believed to support and nourish the body’s nerves.
External influences like wind, cold, or dampness may also disrupt the body’s internal balance, leading to symptoms such as numbness, tingling, or sharp, radiating pain. Instead of targeting only the site of discomfort, TCM aims to correct underlying imbalances and restore smooth, harmonious flow throughout the body.
Treatment for nerve pain in TCM often involves acupuncture to stimulate specific points that promote circulation and healing. Herbal medicine is frequently used in combination, with formulas designed to nourish blood, strengthen the liver and kidneys, and dispel pathogenic factors. Other traditional therapies, such as moxibustion (a warming technique using mugwort) or cupping, may be applied to enhance circulation and relieve tension. TCM practitioners also offer guidance on diet, lifestyle, and emotional health to support the body’s natural healing processes and prevent further pain episodes.
A 2023 meta-analysis of 16 studies involving over 1,000 patients with neuropathic pain found that acupuncture significantly reduced pain intensity compared to sham or no treatment.
Acupuncture can modulate receptors and ion channels in peripheral nerves, reducing spontaneous nerve activity that leads to pain.
Studies have shown that acupuncture stimulates the release of neurotrophic factors like nerve growth factor (NGF) and brain-derived neurotrophic factor (BDNF), which support nerve regeneration and repair.
Acupuncture Near Me for Nerve Pain in West Los Angeles
If you’re struggling with nerve pain and looking for a natural, holistic approach to healing, acupuncture and Traditional Chinese Medicine may offer the relief you’ve been hoping for. At Art of Wellness Acupuncture in West Los Angeles, we specialize in helping patients manage complex, chronic pain conditions by addressing the root causes—not just the symptoms. Whether your nerve pain stems from an injury, a chronic condition, or something undiagnosed, we’ll work with you to develop a personalized treatment plan that supports your body’s natural healing processes. Don’t let nerve pain control your life—reach out today to schedule a consultation and take the first step toward lasting relief.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.
How to Treat Watery Eyes With Acupuncture and TCM
By Qineng Tan, L.Ac., Ph.D. and Xiaomei Cai, L.Ac., Ph.D.
Watery eyes, also known as excessive tearing or epiphora, can be a frustrating and uncomfortable symptom, especially when paired with itchiness, redness, burning, or blurry vision. For many people, this problem flares up seasonally due to allergies, while others deal with chronically runny eyes year-round.
In Traditional Chinese Medicine (TCM), watery eyes are a signal that the body is out of balance. Acupuncture and Chinese herbal medicine can help relieve discomfort, and get to the root cause of why your eyes won’t stop watering.
What Causes Watery Eyes?
Watery eyes can stem from a variety of different health issues, ranging from environmental factors to chronic conditions. Some of the most common causes of water eyes include:
- Seasonal allergies (allergic conjunctivitis) – One of the most common causes of itchy, watery eyes, especially in spring (hay fever) and fall. Pollen, grasses, and other airborne allergens trigger inflammation in the eyes.
- Dry eye syndrome – Ironically, overly dry eyes often produce excess tears as a reflex.
- Blocked tear ducts – A blockage in the tear drainage system causes tears to back up and spill over the lower eyelid.
- Eye infections – Pink eye (conjunctivitis), blepharitis (inflammation of the eyelid), or other infections can trigger watery discharge.
- Irritants – Smoke, wind, strong odors, dust, or chemical exposure can cause the eyes to tear up.
- Aging – Tear production and drainage efficiency change with age, increasing the likelihood of both dry eyes and tearing.
- Eyelid problems – Conditions like ectropion (outward-turning eyelid) or entropion (inward-turning eyelid) can interfere with proper tear drainage.
- Autoimmune disorders – Conditions such as Sjögren’s syndrome can affect tear glands and eye moisture.
- Refractive surgeries or contact lens irritation – These may alter tear film stability or increase sensitivity.
Conventional Treatment for Watery Eyes
In Western medicine, diagnosing watery eyes typically involves an eye exam with a focus on tear production, drainage, and any signs of irritation or inflammation. Tests may include a Schirmer test to measure tear production,Fluorescein staining to assess eye surface health, and/or dye tests to evaluate tear duct function.
Treatments depend on the underlying cause and may include:
- Antihistamines or corticosteroid eye drops for allergies
- Artificial tears or lubricating drops for dry eye syndrome
- Warm compresses and eyelid scrubs for blepharitis
- Antibiotics for infections
- Surgical procedures to correct blocked tear ducts or eyelid malposition
While many people find temporary relief through these treatments, they may not always resolve chronic watery eyes or recurring eye infections. Acupuncture and Traditional Chinese Medicine can offer another, more holistic approach.
TCM Theory – Root Causes of Watery Eyes
In Traditional Chinese Medicine, the eyes are known as “the windows of the Liver.” This doesn’t refer to the physical liver as we usually think of it in Western anatomy, but rather the Liver organ system in TCM theory, which is responsible for storing blood and ensuring the smooth flow of Qi (vital energy) throughout the body.
The Liver is closely connected to the eyes, so any imbalance in Liver Qi or Liver Blood can show up as eye issues—blurriness, dryness, sensitivity, itchiness, or excessive tearing.
Other contributing factors may include:
- Liver Wind or Liver Heat – These patterns can manifest as itchy, red, or irritated eyes, often seen with allergies.
- Kidney Yin Deficiency – When the body’s fluids are deficient, this can lead to dry eye syndrome with reflex tearing.
- Spleen Qi Deficiency – Leads to poor fluid transformation, which may cause congestion or excess dampness.
- External Wind or Heat pathogens – Allergens or environmental irritants can invade the body and disrupt the balance of the organ systems, causing acute symptoms like watery, itchy eyes.
Can Acupuncture Help Watery Eyes?

A TCM practitioner will take a thorough health history and examine your tongue, pulse, and symptoms to determine the root cause of your watery eyes. A treatment protocol may include acupuncture to balance Liver Qi, clear Wind and Heat, and improve fluid metabolism, Chinese herbal formulas to nourish Liver and Kidney systems or clear Dampness and Heat, and dietary therapy to reduce phlegm or support Yin and Blood.
Your acupuncturist will also recommend dietary adjustments that can help clear excess liver heat, such as mung beans, dark, seaweed, arugula, celery, grass fed beef and liver, organic fertile eggs, flax oil, and sesame seeds.
For liver health, is it usually best to avoid alcohol, fried foods, sugar, processed foods, cashews and peanuts, and nightshade vegetables like eggplant and bell peppers.
A randomized controlled trial examined the efficacy of acupuncture in treating dry eye syndrome, a condition that can paradoxically cause reflex tearing. Participants receiving acupuncture reported significant improvements in tear film stability and symptom relief compared to the control group.
A clinical study published in the Journal of Traditional Chinese Medicine investigated the effects of acupuncture on 34 patients suffering from epiphora due to lacrimal duct dysfunction. The treatment involved specific acupuncture protocols aimed at restoring proper tear drainage. The results indicated significant improvement in symptoms, suggesting that acupuncture can be an effective non-invasive treatment for certain types of excessive tearing.
By restoring balance to the underlying systems involved—especially the Liver—TCM not only helps reduce excessive tearing but can also address related symptoms like eye fatigue, itching, redness, and even headaches.
Acupuncture Near Me for Watery Eyes in West Los Angeles
If you’re struggling with constant tearing, itchy eyes, or other irritating symptoms related to allergies, dry eyes, or sinus issues, acupuncture and Traditional Chinese Medicine may offer the relief you’ve been looking for. At Art of Wellness Acupuncture in West Los Angeles, we take a whole-body approach to treating eye conditions by restoring balance and improving circulation through personalized acupuncture treatments and herbal support. Whether your symptoms are seasonal or persistent, don’t hesitate to reach out for a consultation.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.
How to Treat Ovarian Cysts With Acupuncture and TCM
By Xiaomei Cai, L.Ac., Ph.D. and Qineng Tan, L.Ac. Ph.D.

Sharp pain lower abdomen? Feeling bloated or heavy? Pain during intercourse? These can all be signs of an ovarian cyst. Acupuncture and TCM can help relieve pain in lower left abdomen or sharp pain lower right abdomen, while also addressing the root cause of ovarian cysts.
Ovarian cysts are fluid-filled sacs that develop on or within an ovary. These cysts are quite common and often form naturally during the menstrual cycle. While many ovarian cysts are harmless and resolve on their own without causing symptoms, some can lead to pain and may indicate underlying health issues.
TCM has centuries-old methods of helping to regulate women’s hormonal health and offers natural solutions for reproductive care, especially focusing on ovarian health.
Symptoms of Ovarian Cysts
Many people may have ovarian cysts without knowing it, because they do not always cause painful symptoms. However, sometimes a cyst can cause a lot of pain, or may cause pain and bloating that comes and goes during different phases of the menstrual cycle, or due to other factors.
- Pelvic Pain, dull or sharp ache in the lower abdomen, often on one side: ache in lower left abdomen, lower left hand abdominal pain, pain in lower right abdomen.
- Bloating, feeling of fullness or heaviness in the abdomen.
- Pain During Intercourse, discomfort during sexual activity.
- Menstrual irregularities, unusual bleeding patterns, including heavier or lighter periods
- Frequent urination, increased urge to urinate due to pressure on the bladder.
- Constipation, difficult bowel movements.
- Nausea, vomiting, especially if a cyst causes the ovary to twist (ovarian torsion)
Ovarian Cyst Diagnosis and Treatment

In Western medicine, ovarian cysts are typically diagnosed through a pelvic examination followed by imaging studies such as ultrasound, which helps determine the cyst’s size, shape, and composition. Additional tests like blood work may be conducted to assess hormone levels or rule out malignancy.
Sometimes the ovary and/or fallopian tube becomes twisted and is pulling on surrounding tissues; this is called ovarian torsion. This cuts off circulation to the ovary, which not only can cause severe pain, but can lead to the “death” of the ovary. This is a serious condition, which requires surgery to untwist or remove the ovary and sometimes the fallopian tube.
When there is no ovarian torsion, the treatment for a cyst will usually involve a wait and see approach, monitoring the cyst over time to see if it resolves naturally, especially if it’s small and asymptomatic.
Hormonal contraceptives may be prescribed to prevent the formation of new cysts, though they won’t shrink existing ones.
In cases where cysts are large, persistent, or causing significant discomfort, surgical removal may be recommended. Procedures range from minimally invasive laparoscopic surgery to more extensive laparotomy, depending on the cyst’s characteristics and suspicion of malignancy.
TCM and acupuncture offer alternative approaches to treating ovarian cysts, focusing on restoring balance.
Can Acupuncture Help Ovarian Cysts?

If you are experiencing serious pain in the left lower quadrant or right lower quadrant, it is important to seek urgent medical care and diagnostics, because ovarian torsion can, in some cases, lead to a rupture and even possibly life-threatening sepsis.
However, in many cases, an enlarged cyst can be helped with complementary therapy with acupuncture and other TCM treatment for cysts.
In TCM, we do not just look at treating the symptoms of a cyst that has already formed. We dig deeper to look at the reasons why cysts are developing on the ovaries. Acupuncture offers a multifaceted approach to treating ovarian cysts by addressing underlying imbalances and promoting the body’s natural healing processes.
A comprehensive treatment protocol for ovarian cysts may include:
- Electro-Acupuncture: By identifying the precise location of the cyst through palpation or medical imaging, practitioners can apply electro-acupuncture directly to the affected area. This involves inserting needles into specific abdominal and lower back points and administering electrical stimulation for approximately 30 minutes, aiming to reduce the cyst’s size and alleviate associated symptoms.
- Meridian Point Stimulation: Targeting points along the Liver and Gall Bladder meridians helps to relieve stagnation and promote the smooth flow of Qi. Additionally, points will be used to address dampness and phlegm accumulation, which are often associated with cyst formation.
- Auricular Acupuncture: Placing a tiny seed or needle to target acupoints in the ear can help support reproductive organ health and balance hormonal levels.
In addition to acupuncture, Chinese herbal medicine plays a crucial role in the treatment of ovarian cysts. Specific herbs are known for their properties in invigorating blood circulation and resolving phlegm stagnation. These herbs can be integrated into formulas tailored to the individual’s specific pattern of disharmony, considering factors like Spleen dampness, Liver Qi stagnation, and internal heat.
Implementing lifestyle modifications is also essential in managing and preventing ovarian cysts. Your acupuncture practitioner will talk with you in-depth about dietary changes that may help combat Spleen dampness. Meditation and movement practices like Qi Gong and Tai Qi can help alleviate stress and promote the smooth flow of Qi. Some simple changes in physical habits, like crossing the legs or walking with pronated feet can help with contribute to Qi stagnation in the pelvic region.
By integrating these acupuncture techniques, herbal remedies, and lifestyle adjustments, Traditional Chinese Medicine offers a holistic and individualized approach to treating ovarian cysts, aiming to restore balance and promote overall reproductive health.
Acupuncture Near Me for Ovarian Cysts in West Los Angeles
Acupuncture treatment can help relieve the pain of ovarian cysts as well as help balance hormones and organ system health, so that cysts don’t keep coming back again. If you are experiencing any menstrual pain, PCOS or infertility issues, please do not hesitate to come in for a consultation. Dr. Cai is a reproductive health specialist, with training in both TCM and Western gynecological medicine. She has helped many hundreds of people here in Los Angeles with women’s health issues of all kinds.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.