-
 Art of Wellness Acupuncture & Traditional Chinese Medicine (TCM)11704 Wilshire Blvd, Suite 295, Los Angeles, CA, 90025
Art of Wellness Acupuncture & Traditional Chinese Medicine (TCM)11704 Wilshire Blvd, Suite 295, Los Angeles, CA, 90025
myartofwellness@gmail.com310-451-5522 Office Hours
MonClosedTue7:30 am --4 pmWed7:30 am --4 pmThu7:30 am -- 4 pmFri7:30 am -- 4 pmSat7:30 am -- 4 pmSunClosedOur office opens from Tuesdays to Saturdays 7:30 am to 4 pm, will be closed on Memorial day, Independent day, Labor day, Thanksgiving day, Christmas and New year.
-
Recent Posts
- How to Treat Rosacea With Acupuncture and TCM
- How to Treat Perioral Dermatitis With Acupuncture and TCM
- Lymphatic Drainage With Acupuncture and TCM
- How to Treat Turf Toe With Acupuncture
- How to Treat Nerve Pain With Acupuncture and TCM
- How to Treat Watery Eyes With Acupuncture and TCM
- How to Treat Ovarian Cysts With Acupuncture and TCM
- How to Treat Dystonia With Acupuncture and TCM
- Can Acupuncture Help Bad Breath?
- How to Treat Atopy with Acupuncture and TCM
- Plantar Fasciosis Treatment With Acupuncture and TCM
- How to Protect Yourself When Air Quality Is Poor
- How to Treat Spinal Headache With Acupuncture and TCM
- How to Treat Sarcoidosis With Acupuncture and TCM
- How to Treat Flu With Acupuncture and TCM
- Chinese New Year 2025 Year of the Snake
- Sign up to receive news and updates and get my free report:“The Top 10 Reasons to Try Acupuncture”

July 2025 M T W T F S S 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31
Menopause
How To Treat Frozen Shoulder With Acupuncture and TCM
By Qineng Tan, L.Ac., Ph.D. and Xiaomei Cai, L.Ac., Ph.D.

Can’t lift arm up? Front shoulder pain? Shoulders hurt when sleeping? Shoulder pain that doesn’t go away can be due to “frozen shoulder” and adhesive capsulitis. Acupuncture and TCM offer treatment for adhesive capsulitis frozen shoulder.
What Is Frozen Shoulder? Understanding Shoulder Pain and Adhesive Capsulitis
Frozen shoulder, medically known as adhesive capsulitis, is a painful condition that limits the range of motion in the shoulder. Over time, the shoulder joint can become stiff and difficult to move, leading to a significant loss of mobility.
Frozen shoulder typically progresses through three stages:
- Freezing – pain becomes gradually more intense, and range of motion decreases, sometimes until the arm is immobile – can last 6 weeks up to 9 months
- Frozen – pain may lessen, but the shoulder joint is still stiff and very difficult to move – can last 4-6 months
- Thawing – movement and strength is slowly regained – typically lasts anywhere between 6 months to 2 years
While frozen shoulder may be considered resolved when the pain has improved and basic functionality returns, many people continue to feel some stiffness and pain for many years.
What Causes Frozen Shoulder?
The shoulder is a ball-and-socket joint made up of three bones:
- The humerus (upper arm bone)
- The scapula (shoulder blade)
- The clavicle (collarbone)
The ball of the upper arm bone fits into a shallow socket in the shoulder blade, and this joint is surrounded by a thick capsule of connective tissue called the shoulder capsule. To help the shoulder move smoothly, synovial fluid lubricates the joint.
In cases of frozen shoulder, this capsule thickens and becomes stiff, with the development of adhesions or scar tissue, reducing the fluid in the joint. This usually leads to significant pain and often severely limited movement in the shoulder.
What Are the Risk Factors for Adhesive Capsulitis of the Shoulder?

Frozen shoulder primarily affects adults, especially those between 40 and 60 years old, and it occurs more often in women than men. It is particularly common in women experiencing perimenopause and menopause, likely due to hormonal changes that can contribute to joint and connective tissue issues.
Certain medical conditions increase the likelihood of developing frozen shoulder. For example,
people with diabetes are at a higher risk for frozen shoulder, and they often experience more severe stiffness and longer recovery times.
Both hypothyroidism and hyperthyroidism are associated with an increased risk of frozen shoulder.
Immobilization of the shoulder following surgery or injury can also trigger the onset of frozen shoulder, especially if movement is restricted for long periods.
Many people wake up with a sore shoulder from sleeping in a way that restricts movement. Shoulder discomfort or front shoulder pain can happen due to sleeping positions that put pressure on the sensitive shoulder joint.
Frozen shoulder can also cause discomfort on one side, leading to reports of sore right shoulder or ache in left shoulder depending on which shoulder is affected.
Treatment for Frozen Shoulder/Adhesive Capsulitis
A doctor will typically diagnose frozen shoulder after an examination to determine passive range of motion and active range of motion in your shoulder. They may choose to order X-rays to rule out other problems.
In most cases, using hot and cold therapy with compresses and icing may be recommended, as well as pain medications/anti-inflammatories like Ibuprofen. If pain continues to be severe, a physician may offer steroid injections (corticosteroids).
Patients may be referred for physical therapy or massage to help with stretching and improving range of motion.
If pain and immobility persists past a year, surgery may be recommended. A “capsular release” procedure involves making small incisions in the tissues of the shoulder capsule. Manipulation and massage, while a person is anesthetized, can also help loosen up the tissues to allow for more mobility.
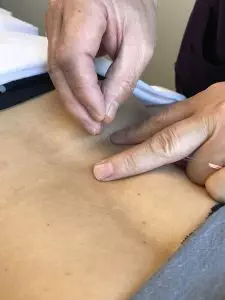
Acupuncture treatment can help relieve pain and improve mobility for frozen shoulder treatment without negative side effects that can come from the ongoing use of OTC pain medication and cortisone shots/corticosteroids, so it may be considered as an adjunct or alternative treatment for adhesive capsulitis.
Can Acupuncture Help Frozen Shoulder?
The TCM Chinese term for “frozen shoulder” translates into English as “shoulder at the age of 50 years.” Clearly, people in their middle age have been experiencing this pain and limitation in the shoulder joint for centuries. TCM has developed ways of helping to improve this condition.

According to TCM theory, frozen shoulder may fall under the category of “Bi Syndromes.” “Bi” refers to an obstruction of some sort, and Bi Syndromes typically cause pain and stiffness in a part of the body, due to a blockage of the flow of Qi (life force energy).
In TCM, “wind,” “damp,” and “cold” are considered pathogenic forces that can settle in an area of the body and cause blood and Qi to stagnate. This can cause stiffness, lack of movements, tenderness, swelling, and pain in that area. Most types of arthritis, for example, are considered Bi Syndromes.
Conventional medicine tends to treat each person presenting with a condition with the same types of treatments and waits to see if they work. In TCM, there is an understanding that different people can have the same symptoms, and yet have different underlying problems that are causing pain and other symptoms.
Different people may experience pain and stiffness due to different factors. One person may have a stiff, sore shoulder due to an invasion of cold or damp, while another person may show signs of heat or wind. In other words, the very specific presentation of symptoms can help the acupuncture practitioner to determine the underlying causes of the condition and treat them accordingly, with acupuncture and herbal remedies.
The stimulation of specific acupoints can help bring more blood flow to the shoulder joint, so that more nourishment can help reduce inflammation. Electroacupuncture, in particular, can help activate the release of endorphins that reduce pain.
A review of 13 controlled studies of the usage of acupuncture treatment for frozen shoulder determined that it is a good modality for both reducing pain and restoring proper shoulder function.
A randomized, single blind controlled trial looked at 35 patients with frozen shoulder symptoms. Some of the patients were assigned to a group that would engage in physical therapy sessions twice per week, practice exercises at home daily, and not use any pain medications, except in “emergency” situations.
The other group also engaged in physical therapy and exercise, plus they also were given acupuncture treatment twice per week, with functional movement exercises being performed during the acupuncture session.
After six weeks of treatment, patients who had only had PT showed an average 39.8% improvement, while the PT plus acupuncture patients showed an average 76.4% improvement.
One recorded case study detailed that, after 24 acupuncture treatments, a patient regained full range of motion in their shoulder and reported that pain was entirely gone.
Acupuncture for Frozen Shoulder Near Me in West L.A. and Santa Monica
At Art of Wellness Acupuncture in West Los Angeles, we have over 35 years of experience helping patients find relief from joint pain of all kinds. Dr. Tan is a specialist in treating orthopedic pain. We successfully treat joint pain conditions like frozen shoulder, osteoarthritis of the knee, tennis elbow, bone spurs, bursitis/hip pain, gout, and more. If you are suffering from a lack of mobility and pain in shoulder, please consider visiting our acupuncture office in Los Angeles for a consultation.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.
How to Treat Diarrhea With Acupuncture and TCM
By Qineng Tan, L.Ac., Ph.D. & Xiaomei Cai, L.Ac., Ph.D.

Chronic diarrhea, explosive diarrhea, diarrhea after eating? Diarrhea may be related to IBS (irritable bowel syndrome), or an IBD (inflammatory bowel disease), or a reaction to a food allergy, parasites, or stress. Acupuncture and TCM offer an alternative diarrhea treatment, so you can get relief from stomach pain and diarrhea.
Why Do I Have Diarrhea?
There can be many different causes of diarrhea, also known as loose stool. Acute diarrhea, which only lasts one or two days, will usually go away on its own.
Watery diarrhea that lasts a few days is usually due to food poisoning. Eating something that was rotten, or not cooked properly to destroy bacteria, can cause vomiting and diarrhea. Watery diarrhea can also happen when you have some type of viral infection, such as the “stomach flu.”
Chronic diarrhea, or persistent diarrhea, which lasts for weeks, or bouts of diarrhea that come and go frequently, may be related to IBS symptoms, IBD symptoms, Celiac disease, SIBO, or some other problem.
More than 6% of adults in the U.S. report having chronic diarrhea. Chronic diarrhea in children is also a serious health concern worldwide.
Top 10 Causes of Diarrhea
Diarrhea is a common condition that everyone experiences sometimes. Usually it is temporary, but it can become persistent and serious enough to require diarrhea treatment. The most common reasons a person experiences loose bowel movements include:
- Bacterial infection, traveler’s diarrhea, food poisoning, unsafe drinking water
- Viral infection, such as rotavirus, viral gastroenteritis, stomach flu
- Parasite infection, such as giardiasis
- Food allergy, food intolerance, food sensitivity, Celiac disease
- Reaction to medications like antibiotics, antidepressants, or Metformin
- Reaction to radiation therapy, cancer treatment
- IBS – diarrhea, constipation, and stomach cramps are common IBS symptoms
- IBD – colitis or Crohn’s disease, inflammatory autoimmune disorders that affect the gut
- Malabsorption of food, poor absorption of nutrients
- Menstrual cycle or Perimenopause – changes in hormones/estrogen can cause diarrhea
Certain foods can cause diarrhea, including: too much coffee, artificial sweeteners like mannitol and sorbitol, and red food coloring. Magnesium supplements can also cause loose stools.
If diarrhea lasts more than a few days, it is important to seek healthcare advice. Chronic diarrhea can lead to dehydration and fatigue, and may be happening because of some more serious condition that needs to be addressed.
What Causes Chronic Diarrhea?

Bouts of diarrhea that keep recurring can be a symptom of disorders such as:
- IBD (inflammatory bowel disease) – the most common IBDs are ulcerative colitis and Crohn’s disease. IBD symptoms usually include bloody diarrhea and abdominal pain. IBDs can cause chronic or recurring diarrhea, which can lead to dehydration, fatigue, and weight loss. IBDs can be mild, or so serious that they cause long-lasting damage to the gastrointestinal tract.
- Ulcerative colitis – an autoimmune disorder that causes inflammation and ulcers, or open sores, in the lower gastrointestinal system, including the colon and rectum.
- Crohn’s disease – an autoimmune disorder that causes inflammation mainly in the small intestine, but can affect any part of the GI tract.
- IBS – Irritable bowel syndrome can seem similar to IBDs, also causing recurring bouts of diarrhea and stomach pain. However, IBS is considered a functional gastrointestinal disorder. It is quite common. People with IBS symptoms may have alternating bouts of diarrhea and constipation. People who tend to have more diarrhea-dominant IBS have “IBS-D.”
- Celiac disease – an autoimmune disorder in which a reaction to eating wheat gluten causes serious inflammation of the GI system, leading to abdominal pain, bloated stomach, diarrhea, malnutrition, fatigue, and skin rashes.
With these conditions, diarrhea is brought on periodically—sometimes alternating with constipation, as in some cases of IBS—by factors having to do with the diet or stress, or with autoimmune processes.
Some surgeries that affect the gastrointestinal organs—like gastric bypass, gastric sleeve, or gallbladder removal—can cause chronic diarrhea.
Chronic diarrhea can be caused by an inability of the intestinal walls to absorb nutrients, and/or of the walls of the colon to absorb liquid. It may also be due to excessive action of the intestine in terms of peristalsis, the squeezing of the intestine to move matter through.
Diarrhea Treatment
Acute diarrhea usually goes away on its own in a day or two. Often, people will use OTC remedies for diarrhea and stomach pain, such as Immodium or Pepto-Bismol.
If you have been experiencing persistent diarrhea and seek medical advice, a doctor will perform tests to figure out what is causing the diarrhea, and will offer electrolyte fluids to help with dehydration. Blood tests or a stool test will show if the diarrhea is due to a bacterial infection or parasitic infection.
If chronic diarrhea is determined to be related to a medication you are already taking, then that may need to be adjusted.
Discovery of IBS or an IBD usually involves more diagnostic testing, including a colonoscopy and/or endoscopy, to see if there is inflammation or blockage in the GI tract.
Medical treatment for IBS may involve being offered antispasmodic medications that relax the intestinal walls and slow down the movement of the bowels and can help relieve stomach cramps and abdominal cramping. Dietary changes and behavioral therapy may be recommended.
Pharmacological treatment for IBDs like colitis and Crohn’s usually involves taking a combination of anti-inflammatories and immunosuppressants, to reduce inflammation in the gut and to block the inappropriate autoimmune responses that are triggering the inflammation. Unfortunately, steroids and medications like Xeljanz can cause other side effects and health problems.
Medical treatment for chronic diarrhea may help relieve symptoms and reduce the frequency of bouts of diarrhea, but it does not necessarily address the underlying causes of diarrhea.
Acupuncture and TCM offer an effective alternative treatment for diarrhea that is more suited to each patient’s individual situation.
Can Acupuncture Help Diarrhea?
Chronic diarrhea, according to TCM theory, is usually considered to be related to the health of the spleen. In TCM, the organ systems all interact harmoniously, unless there is imbalance. The imbalance of one organ system may throw off other systems, leading to various symptoms.
In TCM, the spleen is responsible for breaking down the nutrients from food and converting them into energy. If the spleen is not functioning properly, watery stool is often the result. Diarrhea, stomach pain, and other symptoms may differ from person to person, depending on how the spleen is interacting with the liver, stomach, or kidneys.
Common Chinese Medicine diagnosis patterns for chronic diarrhea include:
- Spleen Deficiency with Liver Qi stagnation: mucus in the stool, abdominal pain, cramping, gassiness, bloated stomach, irritability, and feelings of depression
- Spleen Deficiency with Stomach deficiency: watery stools, poor appetite, feeling full quickly, stomach distended after eating, pallor, and fatigue
- Spleen Deficiency with Kidney Deficiency: diarrhea in the morning, partially digested food in the stool, abdominal pain, lower back pain, knee pain, feeling cold
Acupuncture treatment for diarrhea, which may include moxibustion and herbs, aims to support the health of the spleen and other organs. Acupuncture has been shown to help relieve diarrhea and constipation related to IBS. Acupuncture treatment can also help with reducing stress and anxiety, which are common triggers for IBS symptoms.
Acupuncture can also help with diarrhea due to IBDs like ulcerative colitis and Crohn’s disease by reducing inflammation and helping to balance immune responses. TCM treatment for Crohn’s disease or colitis, incorporating nutrition and herbal supplements, can help improve the gut biome and strengthen the lining of the intestinal walls.
Acupuncture for Diarrhea Near Me, Los Angeles, West L.A., and Santa Monica
TCM treatment with an experienced acupuncturist near me can be very beneficial for anyone dealing with ongoing gastrointestinal distress. Both adults and children can find relief from diarrhea, constipation, stomach cramps, bloating, and abdominal pain related to conditions like IBS, IBDs, or celiac disease through acupuncture and herbs. At Art of Wellness, we have over 30 years of experience helping people with gastric disorders of all kinds.
*This article is for education from the perspective of Traditional Chinese Medicine only. The education provided by this article is not approved by FDA to diagnose, prevent, treat and cure human diseases. It should not stop you from consulting with your physician for your medical conditions. Traditional Chinese Medicine is based on Qi, which is an invisible force that usually cannot be observed by modern science. Because science focuses on testing ideas about the natural world with evidence obtained through observation, these aspects of acupuncture can’t be studied by science. Therefore acupuncture and Chinese herbs are often not supported by double-blind, randomized trials, and they are considered alternative medicine therapies in the United States.